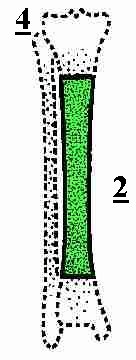
Tibial Fractures
Classification
Descriptive
 |
Site
|
Fracture pattern
|
Displacement
|
Open (Compound) or Closed
Gustilo anderson classification (original 1976, revised 1984)
I
- low-energy with minimum soft-tissue damage, small (<1cm)
wound; typically an inside-to-out puncture. Minimal comminution
of the bone.
II - Laceration 1 to 10 cm long, slight or moderate comminution,
and no or slight periosteal stripping.
III A - Adequate soft tissue cover despite extensive soft-tissue
injury, high-energy trauma, extensive osseous comminution,
segmental fracture
pattern. High risk bacterial contamination eg. Farmyard injuries
included.
III B - Originally defined as fractures with extensive
soft-tissue injury, periosteal
stripping, and exposed bone. Suggest classify III B if
necessitates local or distant flap coverage.
III- C Vascular injury that requires repair for survival of the
limb.
Brumback and Jones 1994 reported interobserver agreement 60 % (range, 42 to 94%)
AO Classification
Tscherne and Gotzen 1984 (soft tissue injury)
0
– Minimal soft-tissue damage, indirect mechanism of injury,
simple bone fracture.
1 - Superficial abrasion or soft tissue contusion caused by
pressure from the bone injury with a mild to moderately severe
fracture pattern.
2 - Deep contaminated abrasion associated with localized skin and
muscle contusion, an impending compartment syndrome, and a
high-energy fracture pattern.
3 – Extensive skin contusion or crushing, underlying severe
muscle damage, a compartment syndrome, and a severe fracture
pattern.
Treatment
General principles
Patients with a closed, stable tibial fracture can be treated successfully with a cast.
Intramedullary nailing is more convenient, and it may provide superior results, but prospective randomized studies with adequate power need to be done to confirm this.
Operative treatment is recommended for open or closed unstable fractures and for fractures that cannot be held in adequate alignment. Intramedullary nail fixation is the treatment of choice for the majority of tibial fractures that require stabilization.
Indications
| Non operative | Operative |
|
|
Treatment Options
Cast treatment
The advantages of cast immobilization over intramedullary nail fixation include a negligible risk of infection, few problems with knee pain, and no need for hardware removal.
Intramedullary nailing
- Reamed
- Unreamed
| Pro’s | Cons |
|
|
Open reduction and internal Fixation ( Plate fixation)
Generally reserved for proximal metaphyseal fractures now. Problems being infection and wound healing.
Recently percutaneous precontoured locking compression plates have become available for very distal tibial fractures.
For Distal Tibial technique manual (click here)
External fixation
Open fractures not amenable to intramedullary nailing, very thin medullary canals, children, or complex periarticular fractures (treated with fine wire frames)
- Monolateral frame
Ring/ fine wire fixator (Ilizarov)
Open fractures (In A & E)
ATLS
(other injuries)
Swab (Some have questioned value)
Photograph
Dressing (saline/ Betadine)
Splint
(If limb deformed and skin under threat, irrigate to remove
macroscopic dirt, reduce and document!! If contaminated bone
reduced into wound no problem as long as inform orthopaedic team
involved in future care)
Antibiotics (choice depends on degree, source of contamination
(grade of injury)
Mainly gram +ve’s - Cephalosporin (Add
Aminoglycoside if suspect gram –ve’s and Metronidazole
if suspect anaerobes) Tetanus prophylaxis
S.
A. OLSON Instructional Course Lectures, The American Academy of
Orthopaedic Surgeons - Open Fractures of the Tibial Shaft.
Current Treatment - J. Bone Joint Surg. Am., September 1, 1996;
78(9): 1428 - 37.
Andrew H Schmidt, Christopher G. Finkemeier, and Paul Tornetta,
III - Treatment of Closed Tibial Fractures - J Bone Joint Surg Am
2003 85: 352-368
BOA guidelines
The Management of Open Tibial Fractures
http://www.boa.ac.uk/PDF%20files/Open%20tibial%20fractures.pdf
RJ Brumback and AL Jones Interobserver
agreement in the classification of open fractures of the tibia.
The results of a survey of two hundred and forty-five orthopaedic
surgeons - J Bone Joint Surg Am 1994 76: 1162-1166.
Interobserver agreement in the classification of open fractures
of the tibia. The results of a survey of two hundred and
forty-five orthopaedic surgeons
RJ Brumback and AL Jones
Orthopaedic Trauma Association, Baltimore, Maryland.
The system of Gustilo and Anderson for the classification of open
fractures is commonly used as a basis for treatment decisions and
for comparison of the published results of treatment. The
reliability of this classification system was tested on the basis
of the responses of 245 orthopaedic surgeons to a survey. The
respondents were asked to provide data about their age, type of
practice, and type of training; the number of open fractures of
the tibia that they treated each year; and their use of the
Gustilo-Anderson classification system. They were also asked to
classify twelve open fractures of the tibia on the basis of a
series of videotaped case presentations. Each case presentation
on the color videotape included demographic data on the patient,
a history of the injury, the results of the physical examination,
the appearance and dimensions of the open wound before the
operation, preoperative radiographs, and selected portions of the
operative debridement with narration. The level of agreement for
the classification of each fracture was determined according to
the largest percentage of observers who chose a single
classification type. The average agreement among the observers
for all twelve fractures was 60 percent. The over-all agreement
for each fracture ranged from 42 to 94 percent. The average
agreement in the subgroup of surgeons who were considered to have
the least experience (residents and fellows) was 59 per cent
(range, 33 to 94 percent).