Thoracolumbar fractures
Introduction
Clinical
Classification
Treatment
Principles
In General
Steroids
Compression fracture
Burst fracture
Flexion Distraction injury
Fracture dislocation
Osteoporotic compression fracture
References
Introduction
Management of thoracolumbar and sacral spinal fractures remains controversial
Early fusion with instrumentation is a generally accepted for unstable injuries with complete neurological deficit; it results in more rapid mobilization, fewer complications, and lower medical costs.
The optimal treatment for patients with mild-to-moderate deformity, an incomplete neurological deficit, and residual spinal canal compromise remains unknown.
Clinical assessment
Suspect spinal injury in high energy trauma
Log roll look for lacerations/ bruising/ swelling, feel for step/ gap
Neurological examination see below grading of injury.
Remember spinal cord terminates inferior border of the L1 vertebral body in adults viz UMN Vs LMN signs
Spinal shock can last 24 to 48 hours ,asses bulbocavernosus reflex. In the absence of this reflex, neurological deficit may be temporary and may not reflect a complete neurological injury.
Sacral sparing, rectal tone and perineal sensation, indicates partial injury and improved prognosis.
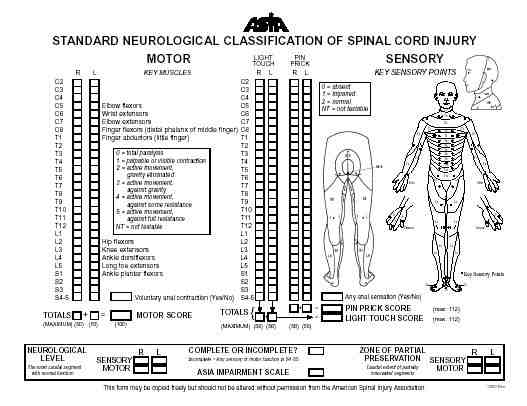
Neurological injury - Grading systems
|
Frankel system (1969)
|
American Spinal Injury Association
(ASIA)
|
Classification and evaluation of spinal stability
Instability - "the loss of the ability of the spine under physiologic loads to maintain its pattern of displacement so that there is no initial or additional neurological deficit, no major deformity, and no incapacitating pain" - White and Panjabi
Possible fracture patterns
- compression fractures
- burst fractures
- flexion-distraction injuries
- fracture-dislocations
Classification of thoracolumbar spine fractures has traditionally been based on theories of spinal stability. Most popular is three column theory of Denis, the two column theory of Holdsworth is making a resurgence
Denis 1984 - 3 column theory
 |
Denis - 3 column classification (1984)
|
The anterior column is formed by the anterior longitudinal ligament, the anterior annulus fibrosus, and the anterior one half of the vertebral body. The middle column is formed by the posterior longitudinal ligament, the posterior one half of the annulus fibrosus, and the vertebral body. The posterior column is composed of the osseous and ligamentous structures posterior to the posterior longitudinal ligament. According to this classification, spinal stability is dependent on at least two intact columns.
Holdsworth 1970 - 2 column theory
The two-column model is one of the earliest models of spinal stability. It is being suggested that the importance of the middle column in terms of long-term stability has been overvalued. Cadaver studies in burst fractures suggest that the integrity of the posterior spinal column provides the greatest resistance to progressive kyphosis and that little additional stability is provided by the middle column.
Holdsworth's anterior column - Anterior longitudinal ligament, vertebral body, intervertebral disc, annulus fibrosus, and posterior longitudinal ligament
Holdsworth's posterior column - Facet joint complex, ligamentum flavum, and interspinous and supraspinous ligaments.
McAfee et al.
Factors indicative of instability
-
Progressive neurological deficit
-
Greater than 20° of kyphosis
-
Greater than 50% loss of vertebral body height
-
Retropulsed bone fragments within the neural canal
Treatment of thoracolumbar fractures
Principles of treatment
Several clinical uncertainties exist in the management of thoracolumbar fractures.
Nonoperative treatment must be considered the preferred method for thoracolumbar fractures in the absence of neurological injury or clear evidence of instability.
In neurologically intact patients, determination of the long-term stability of a fracture is paramount. The integrity of the posterior column is often the decisive factor, and, if the results of the physical examination and the preliminary radiographs are indeterminate, magnetic resonance imaging may be useful.
If stability remains in doubt, a trial of nonoperative bracing with careful follow-up to identify any progressive kyphosis is a reasonable option.
The presence of a substantial neurological deficit suggests spinal instability sufficient to have resulted in injury to the neural elements at the time of the traumatic episode. Some clinicians regard this as sufficient evidence of instability to warrant surgical stabilization, although this opinion remains controversial. Computed tomography or magnetic resonance imaging findings of ongoing canal compromise in the presence of a neurological deficit, however, provide a much stronger incentive for surgical decompression and stabilization.
There is general consensus that progressive kyphosis and progressive neurological loss with evidence of canal compromise due to bone, soft tissue, or an epidural haematoma are strong indications for urgent surgical intervention.
Issues to consider
-
Neurological status - many studies have failed to reveal a substantial difference in functional outcome between operative and nonoperative treatment, regardless of the presence of neurological injury. Most investigators however recommend surgery for patients with progressive neurological injury and significant canal compromise.
-
Stability
-
Degree of deformity
-
Associated injuries
In general
One of the most common clinical scenarios is a compression or burst fracture in a neurologically intact patient with an initial local kyphosis of 25° to 35°. Treatment of such patients should be highly individualized.
Several factors should be considered:
-
Patients age
-
General health
-
Occupation
-
Lifestyle
-
Body habitus
Some investigators have recommended more aggressive surgical treatment for younger patients, with the rationale that fractures in strong healthy bone suggest a higher-energy injury and greater potential for instability. Nonoperative treatment is usually the optimal initial choice in borderline cases, given the ill-defined advantages of surgery in these patients. However, close follow up is mandatory, and evidence of progressive deformity or new-onset neurological deterioration should be addressed by considering surgery.
Steroids
Use of steroids in the management of neurological loss in closed injuries remains controversial suggest follow local spinal protocol
Latest JBJS article advocates steroids use, however the basis for this recommendation the NASICS trials results are disputed by some.
-
Methylprednisolone bolus of 30 mg/kg over one hour followed by infusion of 5.4 mg/kg/hr.
-
If started within 3 hours continue infusion for a total of 24 hours
-
If started between 3 and 8 hours continue for 48 hours
Remember high dose Steroids are not without side effects and the issue is not completely resolved yet.
Compression fractures
Axial loading on a flexed spine. The anterior column fails in compression, middle column remains intact. The posterior column may remain intact or fail in tension, depending on the energy level of the injury. The integrity of the posterior ligamentous structures making up the posterior spinal column is the primary determinant of spinal stability in this fracture pattern.
It is important to ensure it is a wedge compression fracture and not a burst fracture. If in doubt arrange a CT. Using radiographs alone has an error rate of up to 25 %
 |
Compression fractures
Kyphosis angle (Cobb angle)
Posterior vertebral angle
|
Treatment of Compression fractures
Compression fractures are generally stable and rarely associated with neurological compromise.
Less than 40% vertebral body height loss and less than 20° of local kyphosis - Analgesia and early mobilisation
Patients in severe pain despite a stable fracture pattern may benefit from a hyperextension brace
If:
Greater than 40 to 50% of vertebral body height, kyphosis greater than 20° or multiple adjacent compression fractures, the posterior column is subjected to significant tensile force injury and may fail. Progression of kyphosis, compensatory lumbar hyperlordosis, and low back pain may ensue. Treat with either an extension brace or a moulded body cast and regular observation for 3 months.
Operative treatment may be indicated for injuries that have documented progression of deformity despite nonoperative management or when neurological stability is compromised because of the resultant deformity.
Burst fractures
Burst fractures are typically more unstable than compression fractures
and, by definition, involve an injury to the middle column. There is often some
degree of canal compromise, and the risk of neurological injury is
correspondingly greater.
The extent of collapse and kyphosis as well as the integrity of the posterior
column are key determinants of stability and should be considered when deciding
between surgical and nonoperative treatment.
Controversy remains over operative versus non operative management
Progressive neurological deterioration in the presence of substantial canal compromise is an indication for surgical decompression and stabilization
Suggested indications for surgery vary, below are some of those suggested:
- Neurological deficit
- Kyphosis of greater than 15°, 20°, 25°, or 30°
- Greater than 50% loss of vertebral body height
- Multiple contiguous fractures
- 3 column injury
- Multiple injuries
- Open injuries
However, loss of vertebral height, kyphosis, and canal compromise have never been proven in the literature to predict outcome after thoracolumbar burst injury.
Nonoperative treatment of burst fractures
Up to 17% of nonoperatively treated burst fracture patients may develop neurological deficits during treatment. Recent studies have refuted this. For the patient with a stable neurological deficit, nonsurgical treatment may be adequate.
One argument that has been used to promote surgical treatment is that surgery will decompress the spinal canal, preventing the late development of spinal stenosis. Several nonoperative series, have shown spontaneous resorption of retropulsed bone with orthotic treatment.
Another proposed benefit of surgery is prevention of complications associated with prolonged bed rest.
Rechtine et al. compared complications encountered with operative and nonoperative treatment of 235 patients sustaining thoracolumbar injuries. One half of the patients elected nonoperative treatment, which consisted of 6 weeks of bed rest. The overall complication rate was significantly greater in the operative group (31%) than in the nonoperative group (18%) because of an 11% infection rate. Non-wound infection complications were the same between the two groups.
Progression of kyphosis may be encountered with nonoperative treatment. The magnitude of progression, however, has been shown to be from 4 to 7 degrees at follow-up. Furthermore, the degree of kyphosis may or may not correlate with long-term pain or disability.
Burst fractures in neurologically intact patients with less than 50% height loss, less than 20 degrees of kyphosis, and less than 50% canal compromise can be treated nonoperatively.
Treatment
- Bed rest (5 to 10 days)
- Followed by mobilisation in a well-moulded thoracolumbosacral orthosis (3 months)
- Frequent radiographic and neurological examinations to exclude progression.
Operative treatment of burst fractures
There is general agreement that patients with progressive neurological deficits should undergo surgery. In contrast, those patients with complete and stable incomplete neurological deficits, as well as those who are neurologically intact, lack a clearly defined treatment algorithm.
Neurological recovery does not correlate with operative versus nonoperative, only with the degree of initial kyphosis. Patients with greater than 15 degrees of kyphosis at injury showed the greatest neurological recovery. Gertzbein's prospective nonrandomized study of 1019 patients with thoracolumbar fractures demonstrated the benefits of surgery for progressive neurological deficits and decreased pain in the surgically treated group. On the other hand, complications were seen in 25% of surgically treated patients compared with 3% of nonsurgically treated patients. Improvements in techniques of internal fixation reduced the rate and severity of complications in the study
The timing of surgery in the face of neurological deficit is a topic of controversy as well. Gaebler et al., found that those patients operated on within 8 hours had a rate of neurological recovery significantly greater than those treated later after injury. Patients with incomplete injuries had the highest rate of recovery if operated on within 36 hours, and all patients with incomplete injuries had some recovery if operated on within 48 hours. After 48 hours, there was no significant difference between timing of surgery and rate of recovery. Neurological recovery was not correlated with the level of injury (spinal cord, conus medullaris, or cauda equina). This, however, should not be construed as a reason not to operate in a delayed fashion if early surgery is not possible. As Bohlman et al. demonstrated, late anterior decompression is highly effective in alleviating persistent pain and neurological dysfunction secondary to neural compression from thoracolumbar fractures as long as 11 years after injury. Furthermore, McLain and Benson recently reported on urgent stabilization of spinal fractures in polytrauma patients. Patients treated urgently (less than 10 hours after injury) had improved neurological outcomes and similar perioperative complication rates when compared with patients treated at an average of 35 hours from the time of injury.
Flexion-distraction injuries
Flexion-distraction injuries can occur through bone, soft tissue, or a combination of both. Management of “seat belt” injuries is determined by the extent of bony versus soft tissue injury. Isolated injuries through bone, Chance fractures, have a good prognosis for healing. This injury is treated in an extension thoracolumbosacral orthosis for 3 months with frequent follow-up standing radiographs to detect loss of reduction. Flexion-extension radiographs after 4 months of treatment are obtained to assess for fracture healing and potential instability. Surgery is indicated for late instability. Injuries through soft tissue (posterior ligaments, disk) have a more guarded prognosis for healing and may be unstable either acutely or in the long term. These injuries are best treated surgically.
Fracture-dislocations
|
|||
|
Lumbar burst fracture L4 and fracture dislocation L3 on L4 Look carefully at the facet joints (mouseover for detail) |
Fracture-dislocations have the highest incidence of neurological deficit. Patients who are neurologically intact should be surgically stabilized to prevent neurological injury and to permit early patient mobilization. Patients with complete neurological injuries should also be surgically stabilized to hasten rehabilitation.
Osteoporotic compression fractures
These fractures usually follow low energy trauma in elderly patients are and considered separately
References
Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine.1983; 8:817 -31
Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970;52:1534 -51
Ferguson RL, Allen BL Jr. A mechanistic classification of thoracolumbar spine fractures. Clin Orthop.1984; 189:77 -88
Eskenazi, Mark S. Bendo, John A. Spivak, Jeffrey M. Thoracolumbar spine trauma: evaluation and management. Current Opinion in Orthopaedics. 11(3):176-185, June 2000.
K. Wood, G. Butterman, A. Mehbod, T.
Garvey, R. Jhanjee, and V. Sechriest
Operative Compared with Nonoperative Treatment of a Thoracolumbar Burst Fracture
without Neurological Deficit: A Prospective, Randomized Study
J Bone Joint Surg Am 2003 85: 773-781
Alexander R. Vaccaro, David H. Kim, Darrel S. Brodke, Mitchel Harris, Jens
Chapman, Thomas Schildhauer, M.L. Chip Routt, and Rick C. Sasso
Diagnosis and Management of Thoracolumbar Spine Fractures
J Bone Joint Surg Am 2003 85: 2456-2470.