Talus approaches
Indication
Central talar fractures, body and neck
Anatomy
For details of anatomy see talar neck fractures
Bony anatomy
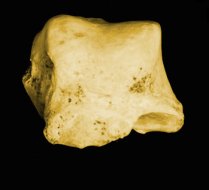
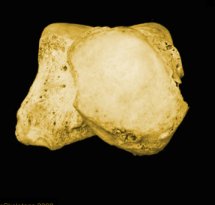 |
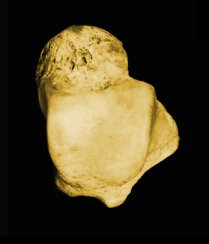 |
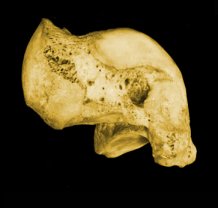 |
| Anterior view | Superior view | Medial view |
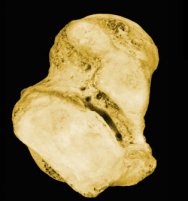
 |
 |
 |
| Posterior view | Inferior view | Lateral view |
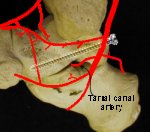
Blood supply
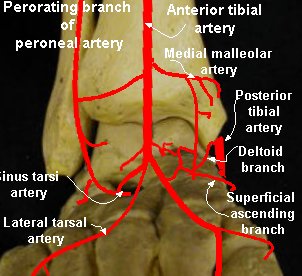
 |
 |
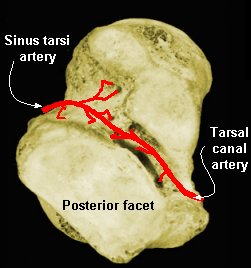 |
|
Medial view - blood supply |
Anterior view - blood supply |
Inferior view - blood supply |
Considerations
Preservation of the blood supply is essential, especially in severely displaced or dislocated fractures.
Several factors affect choice of approach used.
-
Visibility (ability to judge accuracy of reduction)
-
Sparing blood supply
Visibility (accuracy of reduction)
Often two approaches are required to ensure satisfactory reduction and allow for adequate fixation.
The medial malleolus osteotomy should be considered if there is any problem achieving a perfect reduction of the dome or of the posterior process.
The lateral malleolus osteotomy is rarely indicated since moving the foot in maximum plantar flexion generally allows a good view of the anterior half of the lateral side of the dome.
In contrast, maximum dorsi flexion of the ankle gives a good view of the lateral part of the posterior process with a retromalleolar approach.
Where the lateral part of the dome is crushed, the lateral malleolus osteotomy may be useful.
Intraoperative fluoroscopy is mandatory.
It allows checking of the reduction in some “difficult” regions, like the subtalar joints, and testing of the congruency of the joints to be sure that there is no tilting, with the articular surfaces strictly parallel on each side of the joint.
It also allows testing of the correct position and length of the screws.
To demonstrate talar neck - place ankle in equinus, place foot on cassette and pronate 15°, x-ray tube is directed cephalad at a 75° from the horizontal.
Arthroscopy can be useful to check the posterior subtalar joint, to which access is limited.
Sparing the blood supply
Surgical approaches destroy part of the blood supply, and the surgeon should respect the soft tissues surrounding the bone as much as possible.
It
is important to know the anatomical layout of the
blood supply in order to estimate the extent of the
blood supply “sacrifice” according to the supposed
lesions due to the trauma.
For example, on the medial side of the neck, the
anastomosis between the dorsal neck network, the
deltoid branch, and the medial plantar artery branch
are generally destroyed by the anteromedial approach
but sometimes they have to be preserved.
On the posteromedial side, care should be taken of the deltoid branch and of the tarsal canal artery.
From this point
of view, the medial transmalleolar approach is less dangerous for the blood supply than
an extensive
difficult retromalleolar approach.
In the anterolateral approach, one should preserve
at least one of the major sources of the sinus tarsi
network, either from the perforating branch of the
peroneal artery or from the anterior tibial artery.
The lateral transmalleolar approach destroys any
participation of the perforating branch of the peroneal
artery in the sinus tarsi network.
The screws can also destroy the blood supply in the roof of the canal tarsi, particularly if inserted from behind to the lower part of the head.
This could explain the necrosis that can occur, even without dislocation, with a theoretically intact posterior blood supply.
Possible Approaches to Talus
Anterior approach
The anterior approach between the extensor hallucis longus and the extensor digitorum communis is more an ankle approach.
It is deleterious to the blood supply, destroying the main sources of blood supply to the head.
It does not allow any visualisation of the subtalar joints, and is unadapted for correct screw positioning.
This approach should be avoided.
Anteromedial approach
For the anteromedial approach, there are three possibilities:
 |
(1) Along the tibialis anterior tendon, allows good access to the dorsomedial
aspect of the neck and the dome, but with difficult visualisation of the anterior subtalar joint. (2) The lower anteromedial approach, along the tendon of the tibialis posterior, gives a better view of the anterior subtalar joint, but access to the dome is more difficult. To access the anterior subtalar joint, it is helpful to fix a K-wire in the sustentaculum tali to retract the soft tissues. (3) The standard anteromedial approach (solid line) is between the tendons of the tibialis anterior and tibialis posterior. It is a good compromise and it can also be extended by a medial malleolus osteotomy (dotted line), thus giving control over the totality of the medial side of the talus. |
Posteromedial approach
The posteromedial approach is difficult and dangerous.
It is reserved for fractures of the medial side of the posterior process.
The incision is retromalleolar and slightly curved.
The best way to preserve the blood supply of the talus would be behind the neurovascular bundle but generally it is necessary to go close to the tibia, moving the tendons of the tibialis posterior and the flexor digitorum communis.
Any incision of the posterior part of the deltoid ligament should be avoided to preserve the blood supply.
Anterolateral (Ollier) approach
For the anterolateral approach, there are two possibilities:
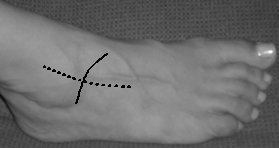 |
(1)The classical sagittal approach (dotted line), follows the lateral side of extensor digitorum longus in front of the lateral malleolus, appears to be the more anatomical one.
(2)The Ollier approach (solid line), oblique from the tip of the lateral malleolus to the neck of the talus, is more effective. Care should be taken of the lateral branch of the fibular superficial nerve at the upper part of the incision. This approach allows better control of the lateral process and the anterior part of the posterior subtalar joint. |
Posterolateral approach
The posterolateral approach is behind the lateral malleolus, between the flexor hallucis longus and the peroneal tendons.
The sural nerve should be preserved and retracted with the anterior side of the incision.
Medial transmalleolar approach
The medial transmalleolar approach could be very helpful in some cases.
It is simple and not deleterious as long as some principles are respected.
Predrill two parallel holes for later fixation.
Then make a chevron osteotomy with
the tip of the chevron a little above the plafond, and the cuts oblique,
descending to the angle between the medial malleolus and the plafond but
incomplete, without penetrating the joint; and then break the last few
millimeters of bone.
Lateral transmalleolar approach
The lateral transmalleolar approach, is more difficult, but seldom indicated.
The fibula can be cut some centimeters above the syndesmosis; then the
tibiofibular as well as the talofibular ligaments are cut, and the lateral
malleolus is moved with preservation of the calcaneofibular ligament.
The reconstruction is made with a plate fixation of the fibula, associated with
ligament repair and syndesmosis fixation.
This technique, which allows perfect
access to the whole lateral part of the talus, seems to be deleterious for the syndesmosis.
To avoid syndesmosis impairment consider osteotomy below.
 |
Cut the lateral malleolus obliquely at the level of the talocrural joint, like a B malleolar fracture, and then cut an anterior triangle with the insertion of the anterior tibiofibular ligament. This preserves the tibiofibular interosseous ligament and the anterior tibiofibular ligament. It is necessary to cut the anterior talofibular ligament to get good exposure of the lateral talar dome. The posterior tibiofibular ligament can be cut, if absolutely necessary, to obtain good exposure of the posterolateral part of the body. Reconstruction is easy, with one or two lag screws and a plate. There is no syndesmosis instability. |
Positioning
Supine
Bring down bed so feet at very end of bed helps with fluoroscopy.
Reduction and fixation
Anatomical reduction
It is necessary to see both sides of the fracture to ensure an anatomical reduction.
 |
With an isolated anteromedial approach the lack of reduction laterally would not be appreciated. |
For neck fractures, one can access the medial half of the neck through an isolated anteromedial approach.
A complementary lateral approach is indicated not only in difficult cases, or where doubt about the accuracy of the reduction exists, but all cases, even so called simple fractures.
On the lateral side of the neck, there is generally a relatively thickened cortical bone spur, which often provides a key to reduction.
With an associated anterolateral approach, it becomes possible to detect two potential flaws, even if it looks “anatomical” on the medial side:
-
An opening of the fracture line (with a loss of contact of the main fragments on the lateral side ie, a varus deformity of the neck)
-
Tilting of the distal fragment in supination or pronation.
These two common malreductions remain generally unsuspected if you perform an isolated approach since they are very difficult to detect on the postoperative x-rays. They strongly impair the function of the subtalar joint.
For joint fractures (body of talus), one is generally satisfied
once the visible part of the dome looks “anatomically”
reduced, often no care is taken to asses
the subtalar joints.
 |
The posterior subtalar joint should be checked by the anterolateral approach.
Where indicated the anterior subtalar joint can be viewed through the anteromedial approach with an incision dividing the anterior part of the deltoid ligament to the sustentaculum tali. The soft tissues can be retracted by a K-wire inserted into the sustentaculum tali. Since direct sight of these joints is not easy, complete checking using fluoroscopy. |
Once an anatomical reduction has been achieved, it is maintained by provisional K-wire fixation.
Care should be taken to avoid secondary displacement when inserting screws.
Aids to reduction
The AO “femoral” distractor can be very helpful, for the reduction of fracture-dislocations and for the exposure of multifragmentary articular fractures.
It is inserted on the medial side with one
pin in the tibia and one through the calcaneal
tuberosity below the neurovascular bundle.
Where a fracture-dislocation cannot be
reduced by hand. Repeated forceful attempts
should be avoided since they increase the
soft tissue damage.
In these cases, the AO distractor can achieve progressive distraction, under fluoroscopic control.
Once the place of the enucleated fragment is recreated by distraction, it is generally easy to reduce the talar body without needing to open the ankle.
For the reduction of multifragmentary articular fractures, distraction generally helps by opening the joints to improve the view inside.
Distraction
by a distractor is more effective than manual traction on a K-wire, or a Schanz pin in the calcaneal
tuberosity as it can be maintained without movement,
allowing precise manouvers on the articular
fragments.
The distraction can be provisionally released when
the reduction of a multifragmentary fracture needs
to press all the fragments against the surface of the
intact corresponding bone, or when mobilization
of the joint is necessary, for instance, in maximum
plantar flexion.
Provisional K-wire transfixation of a mobile posterior fragment through the posterior subtalar joint can be very helpful.
The use of a pointed clamp is not always useful, when pushing the anterior fragment against this posterior fragment as it tends to glide out with a ’soap effect’.
Sometimes, a strong K-wire can be used as ‘joystick’
to correct some tilting of the head and neck fragment in pronation or in supination. This
technique avoids the use of a pointed clamp, which
needs a larger exposure with more damage to the
vessels.
The last tool for helping reduction is
fluoroscopy.
For the subtalar joints in particular, on which direct sight is partial, it is sometimes necessary to achieve reduction by manipulating the joints and the fragments under fluoroscopic control.
Fixation
Screws
Titanium screws should be
used to allow subsequent MRI to detect avascular
necrosis.
Biodegradable screws could be an interesting
future alternative to metallic screws.
Cannulated screws are not as useful as could be expected.
The guide K-wire
cannot be used for provisional fixation. If it is, once
drilled, the fixation
becomes no longer effective and a slight displacement
can occur during screwing. Thus, at least one
other K-wire is absolutely necessary to maintain the
reduction during screwing. In fact, this provisional
K-wire can be used as landmark for positioning a
normal screw. Thus, accurate drilling can be done,
parallel or not to this K-wire, with fluoroscopic control.
The screw is then inserted without any fracture
displacement.
The real need for a cannulated
screws is in (percutaneous) posteroanterior
screwing, which generally can (and should) be
avoided.
Compression is usually needed to achieve strong fixation with an anatomical reduction.
However it should be avoided in cases with comminution.
In such cases, the result of inappropriate compression could lead to shortening of the neck or, worse, tilting of the head and neck fragment, by opening the opposite side.
As a result of these difficulties, lag screws have to be considered with a lot of prudence in the presence of comminution.
If an extrarticular screw is placed into the neck tangentially to bone, the head of the screw comes in contact with the neck early and may displace the distal fragment.
It is sometimes necessary to insert the screws directly into the cartilage of the head, within the talonavicular joint.
Whenever possible, this
procedure should be avoided since this is the most
important joint of the foot. But when absolutely
necessary, it can be done with some precautions.
The head of the screw should always be countersunk,
not only into the cartilage, but also into
the subchondral bone. So, the full thickness
of the cartilage can play a mechanical role above the
head of the screw. In such cases, a 2.7 mm screw is
preferable since its head is smaller.
Another option could be the use of headless
screws.
They do not need any enlargement of the
drilling hole to be positioned in the subchondral bone
and their mechanical properties have been shown to be comparable to those of
“normal” screws.
From the lateral side, insertion of the screw is easy if the fracture runs through the anterior part of the body, leaving intact the anterior part of the lateral process.
In the neck fractures, positioning
of the screw could be more difficult. There is generally a kind of intact strong spur, of the neck in the middle of the anterior
aspect of the lateral process, which allows a
gentle insertion of a small screw.
Therefore, it is generally possible to fix a fracture
of the neck and of the anterior part of the body
with at least two screws inserted from each side in
convergent directions.
The posteroanterior insertion of
screws is exceptionally
indicated in central fractures and is not easy.
There is a narrow place close to the lateral tubercle
of the posterior process, between the groove of
the flexor hallucis longus and the insertion of the
posterior talofibular ligament in the horizontal plane
and between the talocural and the subtalar joints in
the sagittal plane.
The head of the screws should be gently countersunk to avoid any impingement.
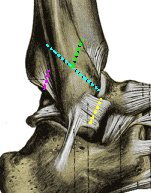
|
There is an increased risk of vascular
injury in the roof of the sinus tarsi if the screw is inserted in the direction
of the lower part of the head. The danger is much greater if the screw is inserted posteromedially, since it destroys the tarsal canal artery close to its origin.
|
Thus, although mechanical tests advocate posteroanterior screwing, which is generally considered safe for the blood supply, it should actually be contemplated with many precautions, and, at least, absolutely avoid the lower half of the head.
Intraoperative reference to a sterile plastic model is useful to choose a safe position for the screws. In all cases, positioning of the screws should be checked by fluoroscopy to detect any problems of length and/or direction. Care should be taken not only of the joints, but also of the roof of the sinus or canal tarsi, to avoid any damage to the blood supply.
K-wires
Normally used for temporary fixation.
Sometimes, it can be helpful to definitely fix some very thin intermediate fragments according to the “lost K-wire” technique.
A small K-wire (0.8—1.0 mm) is “precut” to the estimated length, making a notch, with a usual cutter, at approximately the half of the thickness of the wire. The K-wire is then inserted normally with a motor drive, and once the notch reaches the surface of the fixed fragment, the K-wire is bent laterally and broken.
Therefore, there is no metal sticking beyond the
surface of the intermediate fragment, which can
be then covered by the other main fragment. This
technique should be avoided for the fixation of a
small fragment in an isolated osteochondral fracture,
due to the eventual risk of migration of the
K-wire within the joint.
Resorbable pins are preferable in such cases.
They should be positioned in different directions,
to avoid secondary loosening of the fragment within
the joint.
Plates
Until now plates have been rarely used in talar fractures.
They may be useful in fixing comminuted neck fractures or to fix a malunion osteotomy.
A new AO locked plate that could be used either on the lateral or the medial side is under development.
Osseous graft
A cancellous bone graft is used in cases with subchondral bone loss by impaction, or in comminuted neck fractures.
Subchondral impaction generally involves the dome (especially the posterior part) or the inferior aspect of the head in the anterior subtalar joint.
Usually, part of cartilage remains in
continuity with the intact articular surface as a kind
of hinge, which is helpful.
Reduction is achieved by a gentle leverage
with a spatula or a K-wire, as deep as possible in
the subchondral bone. Cancellous bone chips are
then gently pushed into the bone loss area until the
pressure begins to lift the osteochondral fragment
to the normal level.
Resorbable pins, lost K-wire, or fibrin glue, can
then achieve complementary fixation.
In the comminuted neck fractures with bone loss, the cancellous graft is not used for mechanical properties, but to avoid the interposition of fibrous tissue and then improve the bone healing and the blood supply restoration.
Post operatively
In cases of osteochondral associated lesions, or of articular comminution, use a below knee cast for 4 - 6 weeks.
In the other cases, if stable fixation is achieved,
early postoperative active motion is preferable.
Motion of the joints improves cartilage healing and
motion of the foot improves the blood circulation.
Partial weight bearing is generally allowed after
6 - 8 weeks and total weight bearing after three
months.
In cases of potential or patent necrosis, prolonged non weight bearing cannot be advised.
Long-term immobilization can lead to secondary arthrosis.
References
Injury(2004) 35, S-B10—S-B22; Central talar fractures—therapeutic considerations; Patrick Cronier, Abdelhafid Talha, Philippe Massin