Sacral fractures
Usually consider sacral fractures in conjunction with pelvic fractures.
Unrecognized and inadequately treated sacral fractures may lead to painful deformity and progressive loss of neurological function.
Delayed surgery for posttraumatic sacral deformity is complex, and the results are often less favourable than after early surgery.
Anatomy
Nerves
- Lumbosacral plexus (L4-S1)
- Sacral plexus (S2-S4)
- The anterior rami of S2-S5 contribute to sexual function as well as bowel and bladder control by providing parasympathetic innervation to the bladder and rectum.
- The sympathetic ganglia of the inferior hypogastric plexus extend from the anterolateral L5 and S1 vertebral bodies caudally to the anterior surface of the sacrum along the medial margin of the anterior foramina of S2, S3, and S4.
- The posterior rami of the sacral roots consist of small sensory fibres, with contributions to the cluneal nerves.
Classification
Several classification systems exist - Tile, Denis et al., Roy-Camille et al., Strange-Vognsen, and Isler
Denis three-zone classification system -1988
Based on fracture anatomy
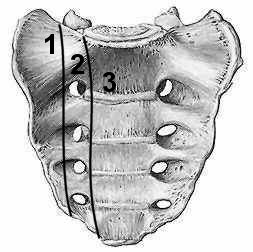 |
Denis - 1988 Zone-I injuries are entirely lateral to the neuroforamina Zone-II injuries involve the neuroforamina but not the spinal canal Zone-III injuries extend into the spinal canal with primary or associated fracture lines |
-
Zone I - Fractures occur lateral to the sacral foramina. The most common, accounting for 50% of the fractures in the series of Denis et al. Zone-I fractures mainly involve the sacral ala, with possible extension into the sacroiliac joint. The fractures can be subdivided into stable and unstable injuries, according to the three-stage severity system. Neurological injury occurs in approximately 6% of patients and typically involves the L4 and L5 nerve roots.
-
Zone II - Vertical transforaminal fracture without involvement of the sacral spinal canal. Second most common pattern, accounting for 34% of the injuries in the study by Denis et al. Neurological injury is found in 28% of patients, and most frequently affects the L5, S1, or S2 nerve root. It is important to distinguish between stable and unstable zone-II injuries because malunions in this area are associated with very poor functional outcomes. Vertical shear injuries are considered to be highly unstable zone-II fractures.
-
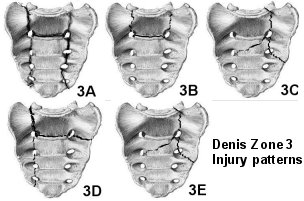
Zone-III - Any sacral fracture involving the spinal canal. Least frequently encountered fracture pattern, only 16% of the patients in the study by Denis et al. Zone III injuries are associated with the highest prevalence and severity of neurological injury. Affecting 57% of the patients.
-
Two additional factors to consider are whether the injury is bilateral and the axial level of the fracture. Patients with a transverse sacral fracture involving the S1, S2, or S3 segment tend to have a higher prevalence of bladder dysfunction than do those with a more caudal sacral fracture affecting the S4 or S5 segment. Bilateral zone-I or II injuries are extremely uncommon and, on closer inspection, are usually associated with an unrecognized zone-III injury with an obscure transverse fracture line.
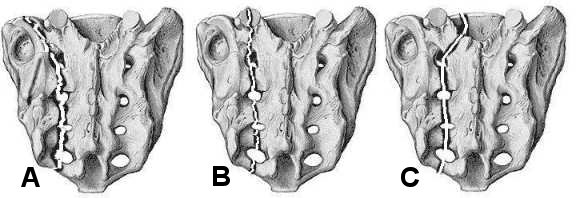
Subclassification of Denis zone-III fractures as suggested by Roy-Camille et al. and modified by Strange-Vognsen
With this subclassification of injury severity, the likelihood of neurological injury, and therapeutic implications are directly related to increasing grade (1 - 4).
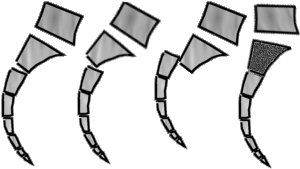 |
Subclassification of Denis zone-III fractures, Roy-Camille et al. - 1985
Modified Strange-Vognsen - 1991
|
Denis Zone 3 injury patterns
 Click
on image for larger image in new window
Click
on image for larger image in new window
Isler - Injury at the Lumbosacral Junction
 |
Lumbosacral junction - Isler 1990 Type A - Lateral to L5-S1 facet Type B - Through the L5-S1 facet joint Type C - Violates the spinal canal. |
| Posterior view |
Lumbosacral Junction
The lumbosacral ligaments are very
strong, patients presenting with an injury in this transitional zone have
usually sustained very high-energy trauma.
Like cervical spine injuries, lumbosacral injuries can be viewed conceptually as
unilateral or bilateral dislocations, with or without accompanying fractures.
Displacement can vary from lumbosacral subluxation to complete lumbopelvic
dissociation. Isler proposed a system for assessing lumbosacral injury on the
basis of the location of the pelvic ring fracture relative to the L5-S1 facet
joint . A vertical sacral fracture lateral to the L5-S1 facet joint
is unlikely to have an impact on lumbosacral stability but may affect pelvic
ring stability. Fractures crossing through the L5-S1 facet joint can be
differentiated as extra-articular fractures of the lumbosacral junction and
articular dislocations with various stages of displacement of the L5 and S1
articular processes. Fractures crossing into the neural arch medial to the L5-S1
joint are usually complex and inherently unstable, necessitating Lumbopelvic stabilization.
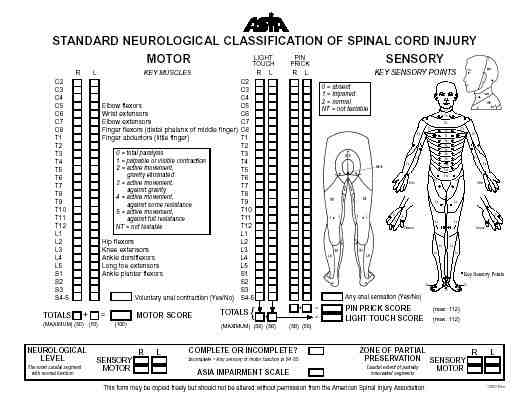
Spinal cord injury classification
Classified in a methodical fashion by the American Spinal Injury Association partly on the basis of the original work of Frankel.
|
Frankel system (1969)
|
American Spinal Injury Association
(ASIA)
|
The systems above, however, incompletely address sacral injuries and the greater variability of neural deficits arising from root injuries.
Gibbons et al. designed a useful four-stage system specifically to grade sacral neurological injuries.
-
Stage 1 - No injury
-
Stage 2 - Parasthesias only
-
Stage 3 - Motor loss but bowel and bladder control intact
-
Stage 4 - Impaired bowel and/or bladder control
Stability
A three-stage system of stability classification has been proposed for sacral injuries.
-
Stage A - Osseoligamentous injury with retention of structural function
-
Stage B - Occult osseoligamentous disruption
-
Stage C - Obvious complete osseoligamentous disruption
Differentiation between Stage-A and B injuries can be very difficult and may require provocative tests, such as weight-bearing and traction studies, or repeated imaging over time.
By convention, any sacral or posterior pelvic fracture-displacement of 1 cm is considered to be unstable.
Clinical
Physical Examination
Approximately 30% of sacral fractures are identified late.
Sacral injury should be suspected in any patient reporting peripelvic pain.
Inspection and palpation of the entire
body is necessary following high-energy blunt trauma, especially in the presence
of an altered sensorium. Lacerations, bruising, tenderness, swelling, and
crepitus are clear signs of a potential underlying injury. More specific signs
suggesting possible sacral injury include a posterior sacral osseous prominence
or a palpable subcutaneous fluid mass consistent with lumbosacral fascial
degloving (Morel-Lavelle lesion).
Patients with a suspected sacral fracture should undergo functional assessment
of the lower sacral roots, including
-
Determination of spontaneous and maximum voluntary rectal sphincter contraction.
-
Light touch and pinprick sensation along the perianal concentric dermatomes of S2 through S5.
-
Specific reflexes - perianal wink, bulbocavernosus and cremasteric reflexes.
All patients with Sacral fractures should have a digital rectal examination and female patients should undergo a vaginal examination to exclude an occult open pelvic fracture.
Pelvic ring stability can be tested manually by gently applied internal and external rotation of the iliac wings. Lower-extremity push-and-pull tests with supplemental radiographic documentation of pelvic shifting have been described but are not commonly performed.
In patients who can walk, the presence of mechanically related low-back or buttock pain may indicate a sacral insufficiency fracture.
Imaging
Radiographs
Due to sacral inclination true AP pelvis not adequate to asses sacral injuries, Pelvic inlet and outlet views improve visualization of the sacrum.
 |
 |
||
|
AP Pelvis |
Pelvic inlet | Pelvic outlet |
Lateral sacrum |
- AP Pelvis - Provides limited visualization of the sacrum due to the inclination angle of the sacrum.
- Pelvic inlet - Shows the sacral spinal canal and a superior view of S1
- Pelvic outlet - Provides true AP visualization of the sacrum.
- Ferguson view - Centrally coned-down modification of a pelvic outlet view directed perpendicular to the sacral inclination to allow en face visualization of the entire sacrum.
- Lateral sacrum - Simple effective radiograph for screening and assessing sacral injuries
Nork et al. identified several radiographic indicators of potential sacral fractures including
- Fracture L5 transverse process (found in 61% of patients with a sacral fracture)
- Paradoxical pelvic inlet view found on supine AP pelvis radiograph (92% of patients)
- Stepladder sign indicative of anterior sacral foraminal disruption
Computed Axial Tomography
CT Scanning is the preferred modality for diagnosing suspected or known posterior injury to the pelvic ring. A dedicated sacral computed tomography scan with 2-mm or thinner cuts as well as sagittal and coronal reformatted views offers superior visualization of a disrupted sacrum and is useful for complex sacral fractures.
Magnetic Resonance Imaging
May be helpful for patients presenting with unexplained sacral neurological deficits after trauma.
Electrophysiological Assessment
Perineal somatosensory evoked potentials and anal sphincter electromyography are useful for assessing patients with a possible neurological deficit related to sacral injury or as a monitoring tool during surgical intervention. Electrodiagnostic evaluation can also be used to differentiate upper motor neuron lesions from spinal cord injury concurrent with sacral trauma or for patients with an injury to the lower part of the urinary tract, for whom neurological evaluation may be difficult.
Cystometrography performed with sphincter electromyography and postvoiding residual measurements can be used as a follow-up test for patients with a neurogenic bladder. However, electromyography is not as useful in the acute setting, as abnormalities may take several weeks to emerge.
Assessment of Sacral injuries
Five basic principles must be followed when assessing a sacral injury.
Presence of active bleeding
Presence of an open fracture
Neurological injury
Pattern and stability of skeletal injury
Systemic injury load
-
Presence of active bleeding: Life-threatening injury to the iliac vessels, anterior perisacral venous plexus, or superior gluteal artery can occur.
-
Presence of an open fracture: Open sacral fractures substantially affects treatment and prognosis. A variant of a true open fracture is an extensive lumbosacral fascial degloving injury similar to that described in Morel-Lavelle syndrome. Technically, these injuries are closed, but it is a substantial challenge to treat them because of the severity of the soft-tissue trauma.
-
Neurological injury: Neurological injury may involve the cauda equina, the lumbosacral plexus, the sacral plexus, and the sympathetic and parasympathetic chains.
-
Pattern and stability of skeletal injury: The issue of defining stability with respect to the pelvic ring remains largely unresolved. Because of the pelvic ring's strong dependence on ligamentous support, any posterior ligamentous disruption of the pelvic ring is likely to be unstable. By convention, any sacral or posterior pelvic fracture-displacement of 1 cm is considered to be unstable. (See Stability above.)
-
Systemic injury load: The cumulative injury load to the patient has considerable short and long-term implications for treatment and outcome. Certain patients or fractures may not be amenable to surgical intervention.
Treatment
Early Management
Early treatment of substantial unstable sacral injuries may include:
-
General resuscitation measures
-
Temporary reduction of a displaced pelvic ring fracture using skeletal traction, application of an anterior external fixator, placement of a pelvic clamp, or use of a wrap-around sheet.
-
Angiographic embolisation of bleeding pelvic vessels if patient remains haemodynamically unstable.
Nonoperative Management
Nonoperative care consists mainly of
activity modification aimed at preventing further fracture displacement. This
may consist of prolonged bed rest in traction, bed rest in a brace, simple bed
rest, or early
mobilization with protected weight-bearing.
The typical time frame for healing of a posterior pelvic ring fracture is 2 to 4
months. This allows for a transitional period of protected weight-bearing of 1 to 2 months.
Remember in all patients on prolonged bed rest:
-
Thromboembolic prophylaxis
-
Pressure care
-
Chest physiotherapy as needed (prevent basal atelectasis)
Repeat imaging studies should be performed to verify that fracture-healing is proceeding with satisfactory alignment.
Progressive fracture
displacement, deterioration of neurological function, or persistent pain with
attempts at mobilization may indicate failure of conservative treatment.
Indications for nonoperative management are vague and historically have included
nearly all sacral fracture patterns. Contraindications to nonoperative care are
relative but include fractures with soft-tissue compromise, an incomplete
neurological deficit with objective evidence of neural compression, and
extensive disruption of the posterior lumbosacral ligaments. Patients with
multiple injuries often benefit from timely surgical intervention in order to
facilitate rehabilitation.
Surgical Decision-Making
Surgical intervention for patients with a sacral fracture should incorporate clear and realistically attainable goals.
Goals include
-
Fracture stabilization and lumbosacral realignment
-
Optimization of the chances for neurological recovery
-
Debridement of open injuries and compromised soft tissues,
-
Minimization of additional morbidity.
Timing of any surgical intervention should be chosen on the basis of treatment goals, the patient's general medical status, and the invasiveness of the surgical procedure. Delayed decompression of neural elements beyond 2 weeks may adversely affect chances for neurological recovery. Most minimally invasive procedures require early closed reduction and are limited in terms of the amount of reduction that is attainable and the overall biomechanical stiffness of the construct. Ultimately, when the treatment is being chosen, the advantages and drawbacks of each approach should be carefully considered.
Neural decompression
Sacral roots subjected to contusion, compression, or traction caused by angulation, translation, or direct compression have a theoretical chance of recovery.
Neural recovery of transected or avulsed sacral nerve roots is unlikely.
Establishing the benefits of decompression over a nonoperative approach in
neurologically impaired patients is difficult. Neurological improvement rates of
up to 80% are frequently quoted, regardless of the type of operative or
non-operative management.
Given an overall rate of neurological improvement of approximately 80%
regardless of treatment, the indications for and timing of surgical
decompression in patients with neurological injuries are somewhat controversial.
From a neurophysiological standpoint, decompression of compromised neural elements is preferably performed early, within the first 24 to 72 hours following injury.
Neural decompression can be achieved indirectly with fracture reduction or directly with a laminectomy. Early surgical decompression may be associated with an increased risk of haemorrhage and wound-healing complications due to soft-tissue contusion and possibly to cerebrospinal fluid leak.
Surgical decompression as an isolated procedure— i.e., without stabilization—is rarely indicated.
Surgical decompression may be less useful in patients with transected sacral roots and reconstruction of root avulsions is impossible.
Traumatically transected roots are commonly associated with Denis zone-III injuries with Roy-Camille type-3 displacement.
Avulsions of the lumbopelvic plexus are associated with severely displaced zone-II injuries (vertical shear injuries).
Surgery should be considered if there is a
reasonable chance of restoring even unilateral lower sacral root function
because such function is sufficient for voluntary bowel and bladder control.
An acceptable approach to early management of sacral injuries is an attempt at
minimal reduction and stabilization. The adequacy of reduction is then assessed
with computed tomography combined with repeat neurological and possibly
electrodiagnostic examination to characterize persistent neurological deficits.
In the presence of satisfactory skeletal stabilization but persistent
neuroforaminal or spinal canal compromise, a focal limited decompression may be
performed within the first 2 weeks after injury, with use of a limited midline
exposure and fluoroscopy-guided focal laminectomy.
Patients presenting with
a severely displaced fracture that is unsuitable for closed reduction and percutaneous stabilization should be considered for a comprehensive posterior
decompression and stabilization procedure with use of the most appropriate
stabilization methods available.
Surgical Stabilization Techniques
Principles
-
Consider anterior pelvic ring stabilization prior to addressing the posterior sacral injury. Methods include, anterior plate fixation, external fixation, or the use of retrograde pubic screws.
-
Ensure stability of the lumbosacral articulation where indicated.
-
Anterior sacral approach, decompression and stabilization has substantial approach-related morbidity and provides limited surgical exposure.
-
Where possible posterior sacral stabilization should offer a high degree of mechanical construct stiffness while producing a low implant profile that minimizes the risk of posterior soft-tissue breakdown.
Posterior sacral stabilization includes:
-
Percutaneous Sacroiliac screws - The vast majority of sacral injuries can be effectively treated with posterior percutaneously based approaches. Percutaneous placement of sacroiliac screws may be contraindicated in patients with anomalous transitional lumbosacral anatomy or when closed fracture reduction cannot be accomplished. Fixation with this method is very challenging in patients with highly displaced zone-II fractures (vertical shear injuries). Zone-II fractures with segmental comminution are susceptible to overcompression and secondary foraminal entrapment when an iliosacral compression screw is used. Such injuries may be considered for fixation with two static sacroiliac screws or for iliolumbar segmental fixation.
-
Open reduction of the posterior aspect of the pelvic ring with plate fixation and screw insertion into the sacral ala, as described by Roy-Camille et al., is an infrequently used strategy.
-
The application of vertically aligned plates on the posterior aspect of the sacral ala with anteroposterior small-fragment screw fixation is also of limited value because of the frequent presence of comminution and osteopenia at the fracture site.
-
Use of a posterior iliac tension-band plate as a supplemental internal fixation method with sacroiliac screw fixation can facilitate open fracture reduction and enhance biomechanical stiffness. However, it requires a posterior two-incision approach, which has been associated with an increased rate of wound-healing complications.
-
The most stable method of lumbosacral fixation involves lower lumbar pedicle screw fixation and iliac screw fixation with longitudanal and transverse connecting rods.
References
Alexander R. Vaccaro, David H. Kim, Darrel S. Brodke, Mitchel Harris, Jens Chapman, Thomas Schildhauer, M.L. Chip Routt, and Rick C. Sasso Diagnosis and Management of Sacral Spine Fractures JBJS - Am., Jan 2004; 86: 166 - 175.
Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop.1988; 227:67 -81.
Roy-Camille R, Saillant G, Gagna G, Mazel C. Transverse fracture of the upper sacrum. Suicidal jumper's fracture. Spine.1985; 10:838 -45
Strange-Vognsen HH, Lebech A. An unusual type of fracture in the upper sacrum. J Orthop Trauma. 1991;5:200-3
Isler B. Lumbosacral lesions associated with pelvic ring injuries. J Orthop Trauma.1990; 4:1 -6.