Lateral cutaneous nerve of thigh
The course of the lateral cutaneous nerve of the thigh is very variable.
It arises from the dorsal branches of L 2 and L3.
It crosses the iliacus muscle deep to its fascia, crosses the deep circumflex iliac artery and enters the anterior region of the thigh by passing under, through, or above the inguinal ligament.
Generally it enters the thigh 1cm medial to the ASIS under the inguinal ligament.
-
Type A - overlies the iliac crest 4%.
-
Type B - ensheathed by the inguinal ligament 27%.
-
Type C - ensheathed by the tendinous origin of the sartorius 23%.
-
Type D - deep to the inguinal ligament and medial to the sartorius 26%
-
Type E, it is positioned medially on top of the iliopsoas 20%. (Aszmann)
Grothaus found it entered the thigh through an opening 36 ± 20 mm (range, 6–73 mm) medial to the ASIS under the inguinal ligament.
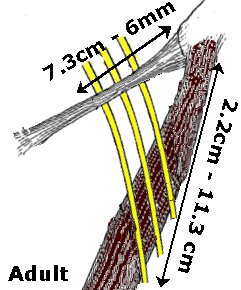 |
In about 30% of the cases, the nerve divides before crossing the inguinal ligament. The nerve then proceeds laterally and crosses the lateral border of sartorius at a variable distance from the ASIS. Generally it crosses the lateral border of sartorius 2.2cm to 11.3cm distal to the ASIS.
|
Crenshaw recommends identifying the nerve as it passes over the sartorius, 2.5 cm distal to the ASIS, and retracting it medially during anterior approaches to the hip.
The LFCN splits into anterior and posterior divisions.
Each penetrates the fascia lata several centimeters below the ASIS.
The anterior branch innervates the area from the anterior thigh to the knee.
The posterior branch supplies the lateral thigh up to the level of the greater trochanter.
Iatrogenic Meralgia Paresthetica
Can occur during
-
Anterior approach to the hip
-
Acetabular fracture surgery
-
Pelvic osteotomies
-
Bone-graft harvesting from the iliac crest
-
Bariatric surgery
-
Laparoscopic hernia repair.
Treatment
Nonoperative
-
Nonsteroidal anti-inflammatories
-
Looser clothing
-
Steroid injection
Resolution of symptoms generally occurs within 3 months.
Persistent symptoms may necessitate surgical intervention.
Surgical options
-
Neurolysis only.
-
Neurolysis and transposition of the LFCN.
-
Transection with excision of a portion of the LFCN. (probably best option)
References
Crenshaw AH: Surgical Approaches: Hip. In Crenshaw
AH (ed).
Campbell’s Operative Orthopaedics. Ed 8. St Louis, Mosby Year Book 58–71, 1992.
Grothaus MC, Holt M, Mekhail AO, Ebraheim NA, Yeasting RA; Lateral femoral cutaneous nerve: an anatomic study. Clin Orthop Relat Res. 2005 Aug;(437):164-8
Aszmann OC, Dellon ES, Dellon AL: Anatomical course of the lateral femoral cutaneous nerve and its susceptibility to compression and injury. Plast Reconstr Surg 1997;100:600–604
Mark G. Grossman, Stephen A. Ducey, Scott S. Nadler, and Andrew S. Levy; Meralgia Paresthetica: Diagnosis and Treatment; J. Am. Acad. Ortho. Surg., September/October 2001; 9: 336 - 344.
Page created by: Lee Van Rensburg
Last updated: 11/09/2015