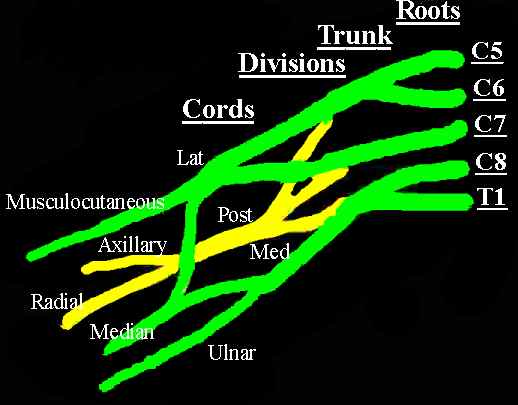
Brachial Plexus
Anatomy
Branches
Supraclavicular
-
Dorsal scapula (C5 frequent contribution C4) - rhomboids
-
Long thoracic (C5,6,7) - serratus anterior
-
Nerve to subclavius(C5 occasional fibres from C4 & C6) - subclavius
-
Supprascapular (C5,6 often also C4) - supraspinatus and infraspinatus
Infraclavicular
Lateral cord (3 branches)
-
Lateral pectoral (C5,6,7) - pectoralis major and via branch to medial pectoral supplies minor (note: called lateral pectoral because from lateral cord, lies more medial than medial pectoral)
-
Musculocutaneous (C5,6,7) - coracobrachialis, biceps brachii, brachialis, ends lateral antebrachial cutaneous nerve
-
Lateral root of median nerve - joins medial root of median nerve to form median nerve
Medial cord (5 branches)
-
Medial pectoral nerve (C8, T1) - pectoralis minor and part of major
-
Medial brachial cutaneous nerve (C8, T1)
-
Medial antebrachial cutaneous nerve (C8, T1)
-
Ulnar nerve (C8, T1 sometimes C7) - Flexor carpi ulnaris, FDP to ring and little fingers, intrinsic muscles of the hand
-
Medial root of Median nerve - joins lateral root of median nerve to form median nerve (see Median nerve )
Posterior cord (5 branches)
-
Upper subscapular nerve (C5,6) - subscapularis
-
Thoracodorasal nerve (C6,7,8) - latissimus dorsi
-
Lower subscapular nerve (C5,6) - also subscapularis and teres major
-
Axillary nerve (C5,6) - deltoid and teres minor
-
Radial nerve (C5,6,7, T1) - triceps, anconeus, brachioradialis, wrist and finger extensors
Brachial plexus injuries
Mostly follow high energy injuries, classically associated with motorcycle
accidents.
Most injuries are closed traction injuries, but direct compression and penetrating injuries also occur.
Male: Female : 8:1
Mechanisms of Injury
- Crush - Caused by direct blunt trauma to the neck and upper extremity, with or without associated injuries. The plexus is crushed between the clavicle and the first rib.
- Traction - This is usually combined with flexion of the neck toward the contralateral side and/or hyperextension of the arm. Caudal traction of the arm will usually affect the upper roots and trunks. Cephalad traction will most likely involve the lower plexus.
- Compression - From hematomas or adjacent tissue elements that have been injured. Delayed compression from Callous in clavicular fractures or subclavian pseudoaneuerysms has been reported.
- Penetrating injury
- Iatrogenic - directly during surgery in the region or compression/ traction in poor patient positioning
In closed injuries the position of the arm in relation to the neck and the trunk, the velocity and magnitude of force applied to the roots and trunks are of great importance. In most cases, these factors determine the severity of the injury and affect the overall prognosis.
Clinical presentation
History
Note carefully mechanism of injury and amount of energy transfer, ask/ look for associated high energy injuries.
Ask about recovery of function. If Horner syndrome noted ask about prior abnormalities of the pupils or eyelids.
Treatment thus far and patients expectations.
Examination
Expose from waist up.
Look
-
At way patient undresses, observe adaption to loss of extremity function.
-
Overall symmetry and obvious scars related to either the initial trauma or subsequent surgery
Feel
-
Palpate supraclavicular and infraclavicular fossae feeling for bony spurs, callus from clavicular fracture.
-
Palpation should also include the ipsilateral chest for diagnosis of fractured ribs. This is important when one contemplates harvesting of intercostal nerves as motor donors for brachial plexus reconstruction.
Move
-
Passive and active ROM of all upper limb joints and neck. Do passive ROM first so joint contracture does not mislead you during motor/ active ROM testing
Neurovascular
-
Document motor power using MRC grading
-
Docuument sensory loss - light touch , two point and moving two point discrimination
-
Tinel sign, tap supraclavicular fossa, a positive sign suggests root rupture as opposed to avulsion. Repeat at subsequent examinations looking for advancement, ie nerve recovery.
-
Examine pulses / perfusion, look for subclavian pseudoaneurysm (palpate, listen for bruit)
-
Consider angiogram if planning brachial plexus reconstruction.
Horner syndrome (meiosis, ptosis and anhydrosis)
-
Positive Hornerís sign implies disruption of the sympathetic supply to the ipsilateral eye and face through the lower roots (C8 and T1) and is a strong indicator of avulsion of these roots.
Radiology
Plain radiographs
-
C-spine - Fractures of the transverse processes might indicate avulsions of the corresponding roots, due to the attachments of the deep cervical fascia between the cervical roots and the transverse processes.
-
Shoulder - Look closely at clavicle and scapula. Fractures of the clavicle and scapula or dissociation of these bony structures from the thorax could indicate a worse supraclavicular injury to the plexus.
-
CXR - Look for fractures of the ribs, because they could indicate injury to the intercostal nerves, a potential source of motor fibres for subsequent neurotization. Inspiration and expiration films or fluoroscopy give information on phrenic nerve function. this is important when considering the ipsilateral phrenic nerve as a motor donor, similarly if going to use the intercostal nerves you want to be sure the phrenic nerve is working.
CT/Myelography
Essentially looking for root avulsions as opposed to ruptures. (pre ganglionic vs post ganglionic)
-
Sensitivity - 95%
-
Specificity 98%
-
Positive predictive value 95%
The main advantage of the CT/myelography is the visualization of pseudomeningoceles, which are usually the result of meningeal tears and subsequent scarring following root avulsion. It is better to perform the myelography at least 1 month after the injury to allow for the pseudomeningocele to be sealed and to prevent the dye from flowing freely to the surrounding spaces. The decision to subject a patient to an invasive procedure such as the myelogram should be made in conjunction with the decision to operate. The cervical CT scan might reveal the absence of rootlets from the corresponding spinal level; this indicates root avulsion. To better use the results of such a study, one should consider that the presence of pseudomeningoceles is strongly indicative of avulsion; however, avulsed roots can exist despite a normal myelogram. Moreover, intact roots can exist in a formed pseudomeningocele if the traction force is strong enough to create a tear in the dura mater but not strong enough to avulse the root from the spinal cord. Because neuroradiology is not pathognomonic, many authors no longer use CT/myelography.
Magnetic Resonance Imaging
MRI has the advantage of good visualization of the brachial plexus beyond the spinal foramen.
On the other hand, good visualization and delineation of the intradural portion of the rootlets are difficult, mainly because of technical deficiencies. Technically, a conventional MRI cannot provide good anatomic depiction of root sleeves and nerves because of the insufficient contrast between the subarachnoid space and the neural structures, a problem caused mainly by cerebrospinal fluid pulsatility. Moreover, correlation of the intradural surgical findings with conventional MRI studies is not reliable in the preoperative diagnosis of root avulsions in 48-52% of patients. This is mainly because of partial root avulsions and intradural fibrosis.
Sensitivity - 81% (up to 89%)
Specificity - 95%
Diagnostic accuracy - 92%
In contrast CT/myelography provides a reliable preoperative diagnosis that correlates with the intraoperative diagnosis in more than 95% of patients.
Electrophysiologic Studies
Axonal discontinuity results not
only in predictable pathologic features but also in time-related electrical
changes that parallel the pathophysiology of denervation. Wallerian degeneration
results in the emergence of spontaneous electrical discharges or fibrillations
that will appear at least 3 weeks after the injury. Therefore, a needle
electromyogram should be postponed for at least that long. In addition to
denervation potentials (fibrillations), a needle electromyogram can also elicit
larger potentials (sharp positive waves). These are valuable when there is a
question whether muscle denervation is complete or if there is some attempt at
reinnervation. Needle electromyogram of the paraspinal muscles, which are
innervated by the dorsal rami of the spinal roots, should also be routinely
performed; denervation of these muscles provides strong evidence of avulsion of
the corresponding roots. On the contrary, if these muscles are electrically
intact, then the injury is most likely infraganglionic and the root is most
likely ruptured. Of course, voluntary potentials in different limb muscles
indicate some neuromuscular continuity. As Bonney and Gilliat demonstrated in
1958, in addition to motor conduction studies, sensory conduction velocities
should also be recorded to differentiate between ruptured and avulsed spinal
roots. If, in a flail anesthetic arm, normal sensory conduction velocities are
elicited, this is a bad prognostic sign that implies root avulsion, which makes
spontaneous nerve regeneration impossible.
Many surgeons find the use of intraoperative somatosensory-evoked potentials
useful to verify a suspected avulsion of a root or to determine whether
resection of a neuroma and interposition nerve grafting should be performed.
The advocates of this intraoperative electrophysiologic technique believe
that root avulsion is definitely excluded only if direct stimulation of the
individual surgically exposed cervical nerve root elicits reproducible
cortical somatosensory-evoked potentials. Others believe that intraoperative
transcranial electrical motor-evoked potentials can be of use in assessing the
connectivity of the roots to the spinal cord.
However, the false positive and false negative recordings are quite high; in
addition, this type of study is time consuming and susceptible to electrical
interferences in the operating theatre.
Treatment
Treatment depends on the nature of injury
-
Nerve root avulsion
-
Nerve root rupture
-
Neuroma/ scarring around nerve
Treatment includes, neurolysis and/or resection of damaged nerve with interposition nerve grafting
Root avulsions carry the worst prognosis and make the reconstruction of the plexus more challenging. A variety of extraplexus donors should be recruited in these cases to reconstruct the distal plexus elements. When the upper plexus roots (C5 and C6) are avulsed from the spinal cord, reconstruction of the shoulder and elbow function can be achieved by means of the C7 root, which can be sacrificed. In that case, the distal targets innervated by the C7 root can be neurotized with extraplexus motor donors. When the three upper roots (C5, C6, and C7) are avulsed, more extraplexus motor donors are needed for reconstruction. Intercostal nerves, if harvested properly, yield acceptable results, especially for reconstruction of the axillary, triceps, or musculocutaneous nerve.
Pain Management in Brachial Plexus Injuries
Injury to the brachial plexus can cause severe pain in about 10- 20% of patients. More common in root avulsions.
Pain usually starts a few days after the pain from the initial trauma subsides and can be intractable. It is commonly described as continuous, burning, and compressing and is frequently located in the hand.
Initial treatment
-
Narcotics
-
Tricyclic antidepressants
-
Antipsychotic drugs
-
Sympathetic blocks.
Limb amputation for control of pain
is controversial, because pain associated with pre ganglionic injury is not
improved by amputation. Early exploration and reconstruction of the brachial plexus, in the majority of
the cases, not only improves the function of the arm but also relieves the postavulsion pain and the pain related to the instability of the shoulder.
References
Terzis, Julia K. M.D., Ph.D.. Papakonstantinou, Konstantinos C. M.D., Ph.D.. The Surgical Treatment of Brachial Plexus Injuries in Adults. Plastic & Reconstructive Surgery. 106(5):1097-1124, October 2000.