Basics of internal fixation
Screws
A screw is a mechanism that produces linear motion as it is rotated.
![]() Synthes screw chart
(PDF file 900kb)
Synthes screw chart
(PDF file 900kb)
Components of a screw
- Head
- Thread
- Shaft
- Tip
Functions of screws
- Fix together 2 or more objects
- Compress objects together (lag, partially threaded screws)
Strength of screw fixation depends on
- Strength of screw material
- Strength of object material
- Design of screw thread
Components of screw in detail
Head of screw
- Stops screw sinking into bone
- Provides connection with screwdriver (allows transfer of torque)
- Shapes - Star, hexagonal, phillips
- Undersurface - normally rounded to provide maximum surface on undersurface after counter sinking and reducing zone of excessive stress which may crack bone.
- Locking screws - have thread on head to allow for locking into plates/ nails, provides angular stability
Diameters
- Core - smallest diameter in thread section
- Shaft - diameter of shaft where no thread
- Thread - diameter of widest part of thread
The strength of a screw is determined by the smallest diameter
The Thread
- Thread shape
- Thread depth
- Thread pitch
Thread shape
- most bone screws have asymetrical threads ie. flat on upper surface and rounded underneath. Providing a wide surface for pulling and little frictional resistance on underside. Increasing transfer of torque to pulling 2 objects together as opposed to simply overcoming friction during insertion
Thread depth
Thread depth is half the difference between thread diameter and core diameter. The amount of thread in contact with bones determines how well screw resists pull out.
ie. In Cancellous bone (weaker than cortical bone ) a deeper thread is needed to capture more material to increase resistance to screw pull out.
Thread pitch
The pitch is the linear distance travelled by a screw for a complete (360º) turn of the screw.
The Tip
- Tapping is the process of cutting a thread, some screws are self tapping
- Some screws may be self drilling self tapping
- Tips, blunt, corkscrew, self tapping, trocar
Pre tapping allows more of the torque applied to be converted into compressing objects together. Prevents bone fragments jamming in thread, increasing frictional resistance and risking damage to bone thread.
Self tapping screws have flutes cut out of screw tip to allow for cuttings to escape.
Cannulated screws
Cannulated screws have a hollow core to allow placement over a guide wire. The hollow core weakens the screw although clinically this is not often a problem.
Types of screw
-
Cortical
-
Cancellous
-
Malleolar
-
Locking - Self drilling, self tapping
The lag screw principle
Allows compression of two objects, screw thread only engages object furthest from head. Can be achieved in two ways:
- Partially threaded screw
- "Lagging" the object closest to the head. By over drilling the near side object to a diameter slightly larger than the thread diameter, creating a gliding hole. The far object is drilled as normal to core diameter and if needed tapped to to the thread diameter. The screw thread only gains purchase in the far object so when the head comes into contact with the nearside object it allows compression of the two objects.
Applications of screws
- Prevent sideways movement
- Hold plate against bone
- Increase grip of intramedullary nail
- Allow axial displacement (eg. dynamic hip screw)
- As part of external fixator assembly
Instruments for inserting screw
Drill bits
- Cutting edges usually 2 may be 3
- Flutes, allow bone cuttings (swarf) to escape
- Direction of drill important, in reverse direction will not clear swarf
Taps
Correspond to thread diameter, shape and pitch of individual screws.
Depth gauge
- Oblique holes may have two depth readings depending on which side measurement made, use longest. A screw hole will only be used optimally if completely filled with a screw.
Screwdrivers
Ensure screw driver not worn and fully seated in head to prevent stripping head of screw.
Screw details
![]() Synthes screw chart
- All diameters of AO synthes screws (PDF file 900KB)
Synthes screw chart
- All diameters of AO synthes screws (PDF file 900KB)
Intramedullary nails
Strength and stiffness
Strength and stiffness of nail depends on:
- Nail diameter
- Materials - Stainless steel, titanium
- Physical characteristics - Solid, hollow, slotted, cross sectional profile
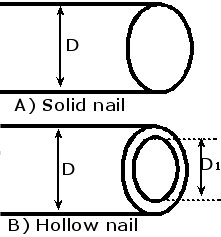 |
Bending stiffness proportional to: A) Solid nail = D4 B) Hollow nail = D4 - D14)
|
Bending strength is proportional to:
D3
Hence as nails get a bit stronger they become considerably stiffer. Very stiff nails may may damage bone on insertion.
Locking
Locking proximally and distally provides rotational and axial stability.
Locking holes may be slots to allow for dynamic compression and shortening while still maintaining rotational stability.
The length of a nail that transmits load from one main fragment to the other is the working length.
The stiffness of a nail in rotation and bending is inversely proportional to its working length.
ie. In a midshaft transverse fracture the working length will be short, enhancing its ability to resist bending and torsional forces.
In contrast a nail across a multifragmentary fracture may rely heavily on the cross locking screws for stability and have a long working length.
The longer the working length the greater the relative movements between the main bone fragments.
Reaming
Intramedullary nails may be inserted in a reamed or un reamed fashion.
Pros and cons exist in use of either nail, each dictated by the clinical situation.
Cross sectional dimensions
Some nails have a clover leaf cross sectional area, thought to allow good contact with bone, whilst preventing excessive nail distortion when twisted
Wall thickness, varies from nail to nail.
Continuous longitudinal slot, allows for flexibility and deformability. Most modern nails are hollow allowing for guide wires and don't have a slot
Plates
Types of plates
-
1/3rd tubular
-
Dynamic compression - DCP
-
Low contact dynamic compression plates - LCDCP
-
Less invasive skeletal stabilization - LISS
-
Locking compression plates - LCP
-
Special plates - Pre contoured plates
Principles of plating
-
Fixation of plates, screws and bone should form as stable a construct as possible
-
Preserve soft tissue and blood supply to bone
-
Place plate in position relative to bone to minimise stress
-
Plate materials should be sufficiently strong to resist fatigue failure
Modes of plating
-
Neutralisation plate - in association with lag screws
-
Compression plate - plate provides compression of fragments
-
Bridge plate - Multifragmentary fracture, plate bridges fracture fragments
-
Buttress
-
Tension band
Neutralisation plates
Screws alone can be used to lag, compress and reduce fractures, however in isolation they are not particularly strong in resisting bending or twisting forces. Here the plate is simply used to neutralise these forces
Compression plating
Dynamic compression plates have specially shaped screw slots with an inclined plane at on end of the slot. As the screw is tightened and as the head engages the slope it slides down the plane shifting the plate relative to the bone.
Bridge plating
In multifragmentary fractures occasionally the only option is to bridge the fracture fragments maintaining alignment and length.
Buttress plating
Usually periarticular, used to buttress up articular surfaces.
Tension band
Bones are not always loaded evenly along all axes. If the fracture is fixed on the side tending to open (tension side) then the tension forces on one side are converted to compression forces on the opposite cortex
How many screws needed in a plate construct?
Depends on individual fractures ability to heal before fatigue failure of plate, screw construct.
ie. Multifragmentary high energy fracture with considerable soft tissue disruption will take longer to heal, making fatigue failure of the implant more likely.
Instead of number of screws better to thing of number of cortical holds
Table below for standard screw plate construct not locking screws
| Humerus | 6-8 cortices |
| Radius and ulna | 6-8 cortices |
| Femur | 6-8 cortices |
| Tibia | 6-8 cortices |
| Fibula, ankle | 6 cortices |
Biological fixation
Absolute anatomical reconstruction needs to balanced with soft tissue preservation minimising periosteal stripping to maximise healing potential.
Intra articular fractures require an anatomical reduction of the joint surface.
Extra articular fractures require mechanical alignment.
MIPO - Minimally Invasive Plate Osteosynthesis, adheres to principle above, intra-articular fractures are reduced anatomically and plates are slipped up under the skin using small incisions and stab incisions for the screws.
LISS - Less Invasive Skeletal Stabilization
External fixation
Types of external fixation
Monolateral frame - Unilateral frames
A or V frame
Ilizarov - fine wire fixator
Hybrid
Unilateral frames
Stability is determined by
-
Frame configuration
-
Degree of contact between bone ends
-
Extent of soft tissue injury
-
Quality of bone pin interface
-
Total number of pins used
The bone pin interface
Bone pins are stiffer than bone itself. The aim is to distribute stresses as evenly as possible to prevent loosening.
Radial pre load - the pin is slightly larger than the pilot hole inducing controlled compression of the bone.
Different companies make different Bone pins/ screws
Orthofix make tapered screws the tip is thinner than the final thickness of the screw.
Available with threads for cancellous and cortical bone.
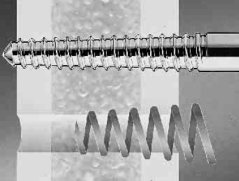 |
This serves two purposes, each thread cuts a new slightly
larger path in the bone and the near cortex thread exerts a radial pre load
on the bone. Similarly it makes removal easier. Care must be taken during
insertion not to insert it too deeply as you cant turn it back a few turns
it looses grip because of the tapered thread. Tapered screws 110/50 6.0-5.0 mm 110 length of pin, 50 length of thread, 6.0 final thread diameter, 5.0 tip thread diameter |
Some bone pins are self drilling self tapping, in principle it is better to drill a pilot hole before insertion in cortical bone.
Recently external fixation pins have been coated with hydroxyapatite, its is said to improve hold, prevent loosening and reduce pin site sepsis.
Orthofix have modified their standard bone pins/ screws, the excaliber range.
-
Single thread design for cancellous and cortical bone - increased threads per unit length increase surface are for contact, with modified profile.
-
Increased stiffness of bone pin
-
The taper has been reduced from 6.0-5.0 mm taper to 6.0 - 5.6 mm, this means you can back out the screw 2 turns without significantly affecting hold, however this is still not recommended.
-
The tip is self drilling, however once again pre drilling a pilot hole is recommended in cortical bone
-
Available uncoated or hydroxyapatite coated.
Insertion of bone pins
Pin size - Greatest diameter of thread should be no more than 30% of bone diameter similarly too small a diameter leads to high loads.
Thread length should be 2-7 mm greater than bone diameter.
Thermonecrosis at insertion sites is thought to lead to increased incidence of pin loosening. Hence pre drilling with a sharp drill and clearing the debri is important.
Working length Distance from fracture to first set of bone pins.