Shoulder Hemiarthroplasty
Trauma
Indication
-
Displaced (Neer) 4 part proximal humeral fractures, with or without associated dislocation of the humeral head.
-
Impression fracture involving greater than 40% of the articular surface
-
Head splitting fractures
-
3-part fracture-dislocations in elderly patients with osteoporotic bone
-
Anatomic neck fractures that are not amenable to internal fixation
Primary hemiarthroplasty is contraindicated in patients whose underlying medical problems preclude surgery. Furthermore, patients who are unable to comply with postoperative rehabilitation should be treated conservatively (ie, alcoholics and uncontrolled psychiatric impairment).
Every attempt must be made at open reduction and internal fixation in younger, active patients.
Anatomy
Blood supply
Main arterial supply to the humeral head is from a branch of the anterior humeral circumflex artery, the arcuate artery.
The arcuate artery ascends on the lateral border of the intertubercular groove and enters the bone at the level of the greater tuberosity, its intraosseous continuation follows a curved posteromedial path, distal to the position of the old epiphyseal plate. Smaller contributions come from posteromedial arteries and, inconsistently, from both the lesser and greater tuberosities. Laing (1956)
Gerber (1990), using selective cadaver arterial perfusions, demonstrated a rich extraosseous anastomosis between the anterior humeral circumflex, posterior humeral circumflex, thoracoacromial and suprascapular arteries, concluding that the anterior circumflex artery was the final common pathway for the supply to the humeral head, and that almost the entire articular surface of the humeral head was exclusively supplied by its intraosseous continuation, the arcuate artery. They found that the posteromedial vessels arising from the posterior humeral circumflex artery supplied only a small inferior articular area adjacent to their site of entry.
Brooks (1993) showed in contrast to the conclusions of Gerber et al (1990), that the humeral head can be completely perfused after ligation of the anterior humeral artery at its site of entry into the humeral head.
They showed a large metaphyseal, epiphyseal anastomosis in six of the eight normal and control specimens.
In long bones with an open growth plate, the epiphyseal and metaphyseal circulations have been described as essentially independent.
Small arteriolar communications are known to develop at the time of fusion of the growth plate.
Brooks et al showed the presence of a large metaphyseal artery which passes through the central area of the fused growth plate to anastomose with the epiphyseal arcuate artery.
This suggests that in the upper humerus at least, the circulations of the epiphysis and metaphysis are not independent.
As regards the management of four-part fractures, these perfusion studies highlight the importance of the posteromedial arteries in maintaining the vascularity of the humeral head.
These vessels pass beneath the humeral capsular attachment, which at this site extends for 1 cm on to the surgical neck, and run towards the humeral head before entering the bone just below the articular margin. After a four-part fracture, when the blood supply from the anterior humeral circumflex artery, the greater tuberosity, the lesser tuberosity and any metaphyseal arterial anastomoses have all been lost, perfusion of the humeral head via the arcuate artery may continue if the head fragment includes part of the medial aspect of the upper part of the neck.
This would explain the findings of Jakob et al (1991) who reported a low incidence of avascular necrosis of the humeral head in four-part fractures in which the humeral head was impacted and in valgus. In this type of fracture the medial aspect of the humeral head is little displaced, and may thus retain its vascularity from the posteromedial vessels.
When the medial fracture line is at the junction between the articular surface
and the neck this anastomosis will be lost and the head will be avascular.
A clear appreciation of the plane and level of all fracture lines is essential
in assessing the remaining blood
supply to the humeral head. CT scanning of the upper humerus with 3-D
reconstruction has been shown to
improve this evaluation in most cases. At open reduction
and internal fixation it is
important to preserve the ascending branch of the anterior humeral circumflex
artery, where this is possible.
If this vessel is disrupted, then the
preservation of soft tissue attachments, especially those containing the
posteromedial vessels, may help to ensure an arterial supply to the head of the
humerus.
The anterior humeral circumflex artery
Is considerably smaller than the posterior, arises
nearly opposite it, from the lateral side of the axillary artery. It runs
horizontally, beneath the Coracobrachialis and short head of the Biceps brachii,
in front of the neck of the humerus. On reaching the intertubercular sulcus, it
gives off a branch which ascends in the sulcus to supply the head of the humerus
and the shoulder-joint. The trunk of the vessel is then continued onward beneath
the long head of the Biceps brachii and the Deltoid, and anastomoses with the
posterior humeral circumflex artery.
The posterior humeral circumflex artery
Arises from the axillary artery at the lower border of the Subscapularis, and runs backward with the axillary nerve through the quadrangular space bounded by the Subscapularis and Teres minor above, the Teres major below, the long head of the Triceps brachii medially, and the surgical neck of the humerus laterally. It winds around the neck of the humerus and is distributed to the Deltoid muscle and shoulder-joint, anastomosing with the anterior humeral circumflex and profunda brachii.
Considerations
Primary hemiarthroplasty for proximal humerus fractures effectively relieves pain.
Functional outcome is less predictable.
Secure tuberosity fixation, restoring the humeral height and retroversion are essential to achieve a good outcome.
Secure and anatomic tuberosity fixation is the limiting factor in achieving
early active motion.
Positioning
Beach chair position sitting up 30 - 40°
The patient's body should be placed at the side of the table so that the humeral shaft can be placed in maximal extension. This will facilitate placement of the prosthesis.
Skin Incision
1. Deltopectoral approach
or
2. Superolateral approach (Mckenzie) - direct better access to tuberosities.
Deep dissection
Identifying the Lesser and Greater Tuberosity
Humeral Stem Preparation and Insertion
Identifying the Lesser and Greater Tuberosity
The biceps tendon is the key surgical landmark.
Once the tendon is identified, follow it proximally and release the rotator interval-between the subscapularis and the supraspinatus.
In a 4-part fracture-dislocation, the lesser tuberosity will be found medially and the greater tuberosity, posterosuperiorly.
The lesser tuberosity should be mobilized from its soft tissue attachments using a combination of periosteal elevators or osteotomes.
In some cases (eg, 3-part fractures), an osteotomy is necessary to complete the fracture. Mobilize the greater tuberosity in a similar fashion.
The rotator cuff should be protected.
A nonpenetrating clamp can be used to capture the tuberosities and mobilize them medially and laterally.
Some authors suggest releasing the long head of the biceps proximally at this point to be tenodesed later.
Humeral Head Retrieval
The head is typically found posteroinferiorly.
It is often helpful to forward elevate the extremity and apply slight distal traction.
Try and remove the head as one fragment to appropriately size the head.
Inspect the glenoid articular surface for damage or wear which may necessitate resurfacing of the glenoid.
Save all bony fragments for autograft later.
Tuberosity Mobilization
Visually estimate the tendinous insertion of the greater tuberosity into thirds and place three #5 nonabsorbable (eg, Ethibond) sutures-superiorly, middle, and inferiorly (sutures #1, #2, and #3, respectively)-from outside-in at the bone-tendon junction of the greater tuberosity.
Similarly, a traction stitch using #5 nonabsorbable suture should also be placed at the bone-tendon junction of the lesser tuberosity.
These steps are critical for later tuberosity reconstruction.
Humeral Stem Preparation and Insertion
Proper placement of the humeral
component at the correct height and in the proper amount of retroversion is
critical to the ultimate stability of the greater tuberosity repair and eventual
outcome of the procedure.
The appropriate humeral height is determined pre- and intraoperatively and then assessed by trial reduction. Placement in proper retroversion is critical to reduce traction on the greater tuberosity repair.
About 20° degrees of retroversion decreases the tension on the tuberosity repair, as described by Boileau et al. This can be achieved by external rotation of the arm to 30° and cementing the component in neutral position.
A helpful landmark is that in this
degree of retroversion, the lateral fin of the prosthesis should lie about 1 cm
behind the distal bicipital groove.
With the trial components removed, drill 2 holes in the humeral shaft, medial
and lateral to the bicipital groove, approximately 1.5-2 cm distal to the
proximal aspect of the humeral shaft.
Pass one #5 nonabsorbable suture from medial to lateral (suture #4) to be used later as a figure-of-eight tension band. Isolate the sutures with a curved clamp and retain the needle.
Pass another #5 nonabsorbable suture (suture #5) through the lateral hole from outside-in.
Retain the needle and grasp the
sutures with a straight clamp.
Prepare and dry the canal. Cement the stem at the correct height and in the
appropriate retroversion.
Place the selected head trial on the stem and reduce the joint.
With tension applied to the tuberosities, assess anterior and posterior stability, as well as range of motion.
Fifty percent translation anteriorly, inferiorly, and posteriorly is desirable.
Check for tuberosity impingement at the extremes of motion.
Once satisfied, remove the trial
head.
Place a looped 2-0 suture without the needle through the medial neck of the
prosthesis. The loop should exit laterally. This will be used later, during the
tuberosity reattachment.
Finally, clean and dry the reverse morse taper, and impact the humeral head implant.
Tuberosity Reattachment
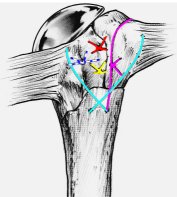
Tuberosity reconstruction is the most important part of this procedure.
The goal is to securely reattach the lesser and greater tuberosity to the shaft as well as to each other.
Consider placing the greater tuberosity approximately 5-10 mm below the superolateral rim of the humeral head component. This is achieved by rigid fixation of the greater tuberosity in proper position, below the humeral head and to the shaft, with a transverse and longitudinal suture.
Next, the lesser tuberosity is fixed to the shaft and the greater tuberosity with sutures through the fin, and finally reinforced with a figure-of-eight tension band suture.
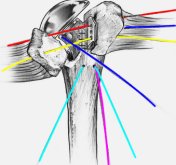 |
First, suture #2 (the middle suture on the greater tuberosity) is placed through the hole located medially on the prosthesis, utilizing the previously placed transport suture. Next, sutures #1 and #3 are passed through the superior and inferior holes on the lateral fin, respectively. Each suture is then passed through the bone-tendon junction of the lesser tuberosity at the corresponding levels.
|
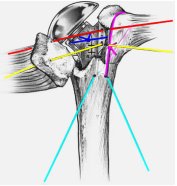 |
Next, pass suture #5,
previously placed longitudinally through the lateral hole in the humeral shaft,
inside out through the superior aspect of the bone-tendon junction of the supraspinatus tendon. Pass this suture under sutures
#1 and #3. The sutures are tied methodically to first secure the greater tuberosity to the prosthesis and humeral shaft. Position the greater tuberosity at the proper height and against the fin of the prosthesis and then tie suture #2 and then suture #5. |
 |
Place bone graft from the humeral head between the tuberosity fragments.
This is followed by securing the lesser tuberosity to the humeral shaft and to the greater tuberosity by tying sutures #1 and #3.
|
 |
Finally, suture
#4 is passed from the supraspinatus through the subscapularis and tied in a figure-of-eight
manner.
At this point, the remaining long head of the biceps may be tenodesed directly to the tuberosity reconstruction. |
The tuberosities should be placed approximately 5-8 mm below the humeral head. Finally, take the shoulder through a range of motion and note the stability of the tuberosities. This will influence the postoperative rehabilitation protocol. Finally, close the wound over a drain and place the arm in a shoulder immobiliser
Exposure extension
Closure
Post operatively
The major risk of early post operative mobilisation is loss of tuberosity fixation.
Rehabilitation depends on the
patient's needs, as well as the intraoperative determination of the security and
tensioning of the tuberosity repair.
Begin active ROM of the elbow, wrist, and hand on day 1 with passive ROM of the shoulder.
Some centres advocate 3 weeks of strict sling immobilization in older, nonactive patients, typically female, with severe osteoporosis.
External rotation is limited based on intraoperative evaluation, and internal rotation is limited to the chest wall.
The patient is discharged from the hospital when he or she is independent in the exercise program and can achieve passive forward flexion of 100 to 120°.
This is generally accomplished within 4 days after surgery.
If this is not achieved, the patient is discharged, and therapy continued on an outpatient basis.
The patient is instructed to use the
sling as needed (6 weeks) but is encouraged to remove it regularly to perform
the exercises several times a day, as well as to use the hand, elbow, and wrist
for simple waist-level activities. Reaching, pushing, and pulling activities are
discouraged for several weeks.
If at 6 to 8 weeks, radiographs show good position and healing of the tuberosities, active ROM can begin. Gentle nonisometric resistance exercises using rubber tubing may commence.
Strengthening and vigorous stretching can be instituted 10 to 12 weeks postoperatively.
Progression of the rehabilitation program is dependent on the patient’s age and
activity level, and will often take 9 to 12 months to reach a maximum level of
improvement.
Results
Primary hemiarthroplasty for proximal humerus fractures typically results in good pain relief with unpredictable functional results.
Several factors adversely affect functional outcome
-
Patients age
-
Postoperative complication requiring reoperation
-
Surgical delay past 14 days
-
Persistent neurologic deficit
-
Tobacco and/or alcohol use
-
Radiographic evidence of failure to restore humeral height or offset
-
Radiographic evidence of retraction of the tuberosities
Robinson et al reported
-
93.9% 10 year overall prosthetic survival rate for primary hemiarthroplasty for the treatment of proximal humerus fractures.
-
Overall median modified Constant score of 64 points, with good scores for pain relief and poorer scores, with greater variability, for function, range of motion, and muscle power.
General results
-
Reported overall good pain relief 90%
-
Forward elevation to 72 - 119°
-
Abduction 101°
-
External rotation to 16 - 40°
-
Internal rotation to theT12 - L2
-
Patients under 70 years of age had significantly greater active range of motion than those over 70.
With respect to tuberosity height, placing the tuberosities too high above the prosthesis will result in impingement and loss of motion. Naranja and Iannotti and others recommend placing the tip of the greater tuberosity 5-8 mm below the top of the prosthetic head. Mighell et al recently reported an average head to tuberosity distance (HTD) of 12 mm for patients with satisfactory, good, or excellent results. However, placing the tuberosities too low (28 mm average HTD) resulted in unsatisfactory outcomes.
Complications
The most common complications following primary hemiarthroplasty for proximal humerus fractures relates to surgical technique.
Failure to anatomically secure the tuberosities, restore the humeral height, and recreate the appropriate humeral retroversion are the most likely reasons for failure.
Overall complication rate has been reported as high as 34%
Complications related directly to the tuberosity reconstruction has been reported as high as 50%.
Infection and neurologic injury are rare complications.
References
Secure Tuberosity Fixation in Shoulder Arthroplasty for Fractures.; Abrutyn,
David A. MD; Dines, David M. MD; Techniques in Shoulder and Elbow Surgery;
Volume 5(4), December 2004, pp 177-183
CH Brooks, WJ Revell, and FW Heatley; Vascularity of the humeral head after proximal humeral fractures. An anatomical cadaver study J Bone Joint Surg Br, Jan 1993; 75-B: 132 - 136
C Gerber, AG Schneeberger, and TS
Vinh
The arterial vascularization of the humeral head. An anatomical study
J. Bone Joint Surg. Am., Dec 1990; 72: 1486 - 1494
Laing PG: The arterial supply of the adult humerus. J Bone Joint Surg Am 1956;38:1105–1116