Lower limb fasciotomy
Indication
Compartment Syndrome lower limb (Tibia).
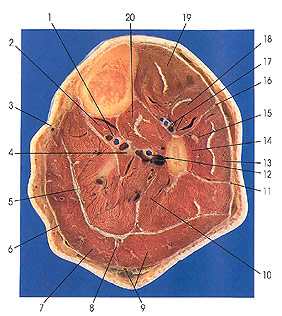
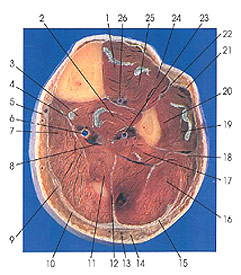
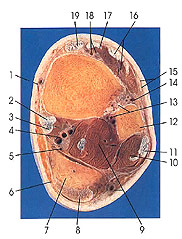
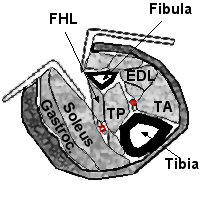
Anatomy
4 Compartments in lower leg (Tibia).
-
Anterior
-
Lateral
-
Superficial posterior
-
Deep posterior
 |
 |
 |
|
UPPER TIBIA
1. Posterior
tibial vessels |
MID TIBIA
|
LOWER TIBIA
1. Great saphenous
v. and saphenous nerve |
Considerations
The lower leg contains four compartments:
-
Anterior
-
Lateral
-
Superficial posterior
-
Deep posterior
The Tibialis posterior muscle sometimes occupies a separate fascial compartment of its own.
Soleus takes origin from the tibia and fibula for the entire proximal half of the leg.
Thus, underneath this “soleus bridge” the deep posterior compartment and its contents are not subcutaneous.
For fasciotomy of the deep posterior compartment, the soleus origin must be detached from either the tibia or the fibula.
Measurement of pressures in the anterior, lateral and superficial posterior compartments are easy.
The pressure in the deep posterior compartment can be measured in the distal half of the leg medial and posterior to the tibia, as it is subcutaneous.
Proximal to this area, the pressure is most easily measured through the soleus origin from the tibia.
Essentially two techniques are possible when undertaking a four compartment
fasciotomy.
-
Perifibular approach (Single lateral incision)
-
Two incision technique
Although subcutaneous fasciotomy may be appropriate in chronic exertional compartment syndromes, it cannot be used for decompression of the deep posterior compartment because this compartment is subcutaneous only in the distal half of the leg.
Positioning
Supine
Skin Incision
The length of skin incision has an effect on fascial decompression in the leg associated with an acute compartment syndrome.
Some authors favour limited incisions, claiming low morbidity, while others recommend long incisions, emphasizing that these are required to decompress affected compartments adequately.
Cohen et al determined the effect of the length of the skin incision in posttraumatic compartment syndromes of the lower extremity treated with fascial decompression using a two-incision technique.
The affected compartments initially were released through 8-cm incisions and the pressures recorded. The skin incisions were enlarged by 2-cm increments until readings showed no further decrease. The final length of the extended incisions averaged 16 cm ± 4 cm.
Mean final pressure in the compartments, which required extension of the incisions, was 13 mm Hg, notably less than pre-extension recordings.
Long incisions add little to
morbidity and influence neither the complication rate nor the late functional
result. Long incisions also eliminate the risk of the skin acting as an
unrecognized compartment envelope, which is especially important during the
hyperaemic period following decompression of an ischemic compartment.
A one- or two-incision approach can be used in the lower leg.
Generally, a long single lateral incision is sufficient for a four-compartment fasciotomy.
Single incision technique
Whitesides described a perifibular single incision technique:
A straight lateral incision just posterior and parallel to the fibula from the level of the fibular head to a point above the tip of the lateral malleolus.
At the proximal end of the incision, the common peroneal nerve should be exposed and/or protected.
The dissection is then deepened to incise the fascia between the soleus and the flexor hallusis longus distally and is extended proximal to release the soleus origin from the fibula.
This allows access to the entire length of the superficial posterior and deep posterior compartments.
The incision should be made long, as decompression of the deep posterior compartment is more difficult with this dissection than with dissection from the medial side.
The anterior edge of the incision is then retracted to expose the anterior and lateral compartments, taking care to avoid the superficial peroneal nerve as it exits the fascia of the lateral compartment and runs anterior in the distal third of the leg.
At the end of this dissection, the
tibialis posterior muscle and others should be checked to ensure that any less
common anatomic arrangement of the compartment is not missed.
Two incision technique
To adequately decompress all four compartments through two incisions, long medial and lateral incisions are required.
Anterolateral incision
Longitudinal incision to expose the contents of the anterior compartment and the lateral compartment, take care to preserve the superficial peroneal nerve distally.
Medial Incision
The location of the medial skin incision is important.
The bulk of the musculature in the superficial posterior compartment is proximal and requires a proximal extent to the incision to adequately decompress the region.
However, the bulk of the deep posterior musculature is located in the distal half of the limb.
The medial incision is made in a longitudinal manner just posterior to the tibia.
The superficial posterior compartment is then opened, and the soleus is detached from its tibial origin to expose the deep posterior compartment in the proximal half of the leg.
In the distal half of the leg, the deep compartment is subcutaneous and can be approached directly.
Adequate decompression requires detaching the soleus origin from the medial aspect of the tibial shaft.
Closure
Sterile/ Vacuum dressing.
Post operatively
Re look ? closure 3 to 5 days.
When muscle necrosis is a possibility, relook at 24-48 hrs.
When the wound edges will not oppose easily, consider split-thickness skin grafting.
References
TE Whitesides and MM Heckman; Acute Compartment Syndrome: Update on Diagnosis and Treatment; J. Am. Acad. Ortho. Surg., Jul 1996; 4: 209 - 218.
Steven A. Olson and Robert R. Glasgow; Acute Compartment Syndrome in Lower Extremity Musculoskeletal Trauma; J. Am. Acad. Ortho. Surg., November 2005; 13: 436 - 444