Forearm fasciotomy
Indication
Compartment syndrome of the forearm
Anatomy
Anatomically, the forearm can be divided into three compartments:
-
-
Brachioradialis, extensor carpi radialis longus and extensor carpi radialis brevis.
Nerve - radial nerve.
-
-
Dorsal - superficial and deep muscles.
-
Superficial - extensor digitorum communis, extensor carpi ulnaris and extensor digiti minimi.
-
Deep - abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, extensor indicis and supinator.
Nerve - posterior interosseous nerve.
Blood supply - posterior interosseous artery and interosseous perforators from anterior interosseous artery.
-
-
Volar - superficial and deep muscles.
-
Superficial - pronator teres, palmaris longus, flexor digitorum superficialis, flexor carpi radialis and flexor carpi ulnaris.
-
Deep - flexor digitorum profundus, flexor pollicis longus and pronator quadratus.
Nerve - median and ulnar nerves.
Blood supply - radial, ulnar, and anterior interosseous arteries.
-
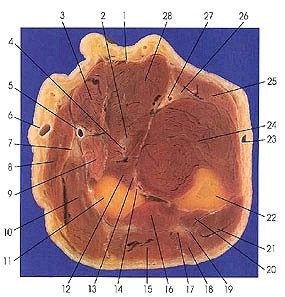 |
1. Tendon m. palmaris longus 2. Median nerve 3. Flexor carpi radialis m. 4. Median a. 5. Radial a. 6. Cephalic v. 7. Radial nerve, superficial br. 8. Brachioradialis m. 9. Pronator teres m. 10. Extensor carpi radialis brevis m. |
11. Radius 12. Flexor pollicis longus m. 13. Anterior interosseous nerve 14. Anterior interosseous a. and v. 15. Extensor digitorum communis m. 16. Abductor pollicis longus m. 17. Radial nerve, deep br. 18. Extensor digiti minimi m. 19. Posterior interosseous a. 20. Extensor pollicis longus m. |
21. Extensor carpi ulnaris m. 22. Ulna 23. Basilic v. 24. Flexor digitorum profundus m. 25. Flexor carpi ulnaris m. 26. Ulnar nerve 27. Ulnar a. 28. Flexor digitorum superficialis m. |
This section passes through the upper middle third of the forearm.
Considerations
Measure compartment pressures in all the compartments of the forearm.
Compartment syndrome is most
common in the volar compartment
but may also develop in the deep aspects
of the compartment, even when the superficial aspects of the
compartment are not involved.
Flexor digitorum profundus and flexor pollicis longus are particularly vulnerable in compartment syndrome, as they may be compressed against rigid bone and the unyielding interosseous membrane.
Most cases of forearm compartment syndrome are adequately treated by release of the superficial volar compartment.
However situations that mandate exploration of the deep volar or dorsal compartments include:
-
High-voltage electrical injury
-
Severe crush injuries
-
Extended extrinsic forearm pressure (such as an unconscious patient lying on his or her forearm)
-
Ongoing evidence of myonecrosis or sepsis despite previous superficial fasciotomy
Some authors consider pronator quadratus to lie within
its own compartment in the distal
forearm,
as elevated tissue pressures can affect it independently from the other forearm
muscles.
Summary
First do a volar fasciotomy.
Repeat pressure measurements in all compartments.
In some cases, tissue pressures in the mobile wad and dorsal compartments will significantly decrease after volar release, making a dorsal fasciotomy unnecessary.
Positioning
Supine arm out on arm table.
+- Tourniquet.
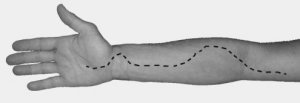
Skin Incision
Volar incision
Several skin incisions have been advocated for exposure.
It has been suggested the straight incision along the ulna border is best as it disrupts less veins and lymphatics.
 |
 |
 |
 |
Dorsal Incision
 |
Line from lateral epicondyle to mid wrist (DRUJ) Extend incision at least to the junction of the middle and distal thirds of the forearm, as most of the musculature is proximal to that point. Do not disrupt the extensor retinaculum of the wrist. |
Superficial dissection
Volar
Routinely release the laceratus fibrosus at the level of the elbow to decompress the median nerve and other structures.
The fascia of the
forearm is then opened from proximal
to distal, exposing the ulnar and
median nerves and opening the superficial
volar muscles as well as
the intervening neurovascular structures.
Pronator teres and flexor
digitorum superficialis may have to
be released distally to complete decompression
of the median nerve in
some cases.
Epimysiotomy is performed on any enveloped muscles.
Do a carpal tunnel release to ensure full decompression.
Dorsal
After completion of the volar decompression, repeat pressure measurements in all compartments, including the dorsal compartment.
In cases in which the dorsal pressures remain elevated, decompress the underlying dorsal compartment.
The standard midline approach can be safely carried deeply between the extensor digitorum communis and the extensor carpi radialis brevis.
Tissue pressures at this point should again be obtained in the deep dorsal compartment and the mobile wad.
A third incision in brachioradialis is rarely required to make certain that it is decompressed.
Deep dissection
When decmopression of the superficial volar forearm is not enough to reduce pressures in the forearm, decompression of the deep structures should be undertaken.
Three standard approaches to the deep volar deep forearm have been described.
Each approach has its own drawbacks.
For example in Henry’s (radial) approach to the anterior radius, the recurrent radial vessels are ligated. Decreasing the blood supply to an ischemic muscle in the context of compartment syndrome could be significantly injurious.
Occasionally the fracture pattern or injury will dictate the approach needed.
Ronel et al showed the ulnar approach caused the least amount of iatrogenic injury to superficial muscles, arteries, and nerves.
Ulnar
Skin incision radial to
flexor carpi ulnaris at the wrist and extended
to the medial epicondyle of the humerus.
Superficial compartment decompressed along the radial side of the flexor carpi
ulnaris, which reveals the ulnar neurovascular bundle.
Flexor carpi ulnaris is retracted ulnarly, and a plane underneath the flexor digitorum superficialis can be appreciated.
As the flexor digitorum superficialis is retracted upward, the median nerve should remain attached to the undersurface of the muscle, radial to its deep belly.
Pronator quadratus can be seen distally between the ulnar neurovascular bundle and the flexor digitorum superficialis; one or two branches from the ulnar artery to the flexor digitorum superficialis may need to be ligated to release pronator quadratus.
Moving proximally, the ulnar neurovascular bundle is raised with the flexor digitorum superficialis to preserve its branches to that muscle.
A branch from the ulnar artery to the flexor carpi ulnaris may need to be ligated.
Raising the flexor digitorum superficialis in the middle third of the forearm allows easy access to the remaining muscles of the deep volar compartment, flexor pollicis longus and flexor digitorum profundus.
Exposure of the three deep muscles allows their evaluation for ischemia and, if needed, individual epimysiotomy.
Central
Skin incision made over the centre of the volar forearm.
Superficial fascia released and the deep dissection continued either radial or ulnar to palmaris longus and then between tendons of flexor digitorum superficialis.
Radial (Henry)
Skin incision radial to the midline of the volar forearm, starting at the proximal wrist crease and extending to the antecubital fossa.
Superficial fascia is released and the dissection continued radial to flexor carpi radialis and between the flexor carpi radialis and the flexor digitorum superficialis.
Exposure extension
Closure
Sterile dressing/ vacuum dressing
Post operatively
Immobilize the arm in a bulky, noncompressive dressing.
Splint the hand. (Edinburgh position)
Delayed skin closure or split thickness
grafting should be done after
appropriate reduction of oedema.
References
TE Whitesides and MM Heckman; Acute
Compartment Syndrome: Update on Diagnosis and Treatment; J. Am. Acad. Ortho.
Surg., Jul 1996; 4: 209 - 218.
Ronel, Daniel N. M.D.; Mtui, Estomih M.D.; Nolan, William B. III M.D. Forearm Compartment Syndrome: Anatomical Analysis of Surgical Approaches to the Deep Space. Plastic & Reconstructive Surgery. 114(3):697-705, September 1, 2004.