Distal tibia trauma Ilizarov
Indication
Temporary external fixation of periarticular fractures of the distal tibia. The option exists to convert it or increase it to definitive fixation as needed. Allows for Limited Open Reduction and Internal Fixation (LORIF), leaving frame in situ.
Perfect for Span and scan of Pilon fractures of the distal tibia
Temporary stabilization of unstable ankle fractures, too swollen for surgery.
Anatomical considerations
See Pin placement below
Calcaneal pins ideally should be inserted as far posterior as possible while still engaging sound bone.
The tendons and neurovascular bundle passing behind the malleoli and the subtalar joint are to be avoided.
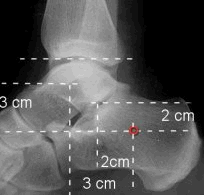
Halett et al suggests for a calcaneal pin place it 2 cm below and behind the lateral malleolus or 3 cm below and behind the medial malleolus BEWARE Tornetta et al show no position is completely safe when placing a medial calcaneal pin or transcalcaneal pin. Ensure you are as far posterior as possible yet still engaging bone.
 |
|
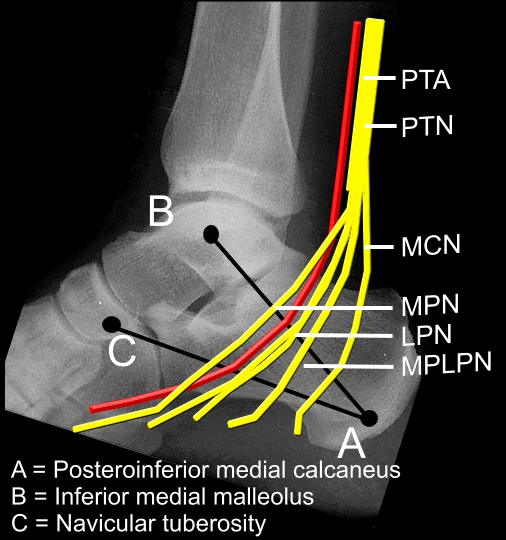 |
The medial calcaneus provides a small window for safe percutaneous
pin placement. A more posterior placement in the safe zone is safest. Careful blunt dissection and the use of cannulas may help to avoid neurovascular injury |
For reasons above use fine ilizarov wires for calcaneal fixation as posterior in calcaneus as possible but still engaging bone.
Positioning
Supine, Radiolucent table
Frame
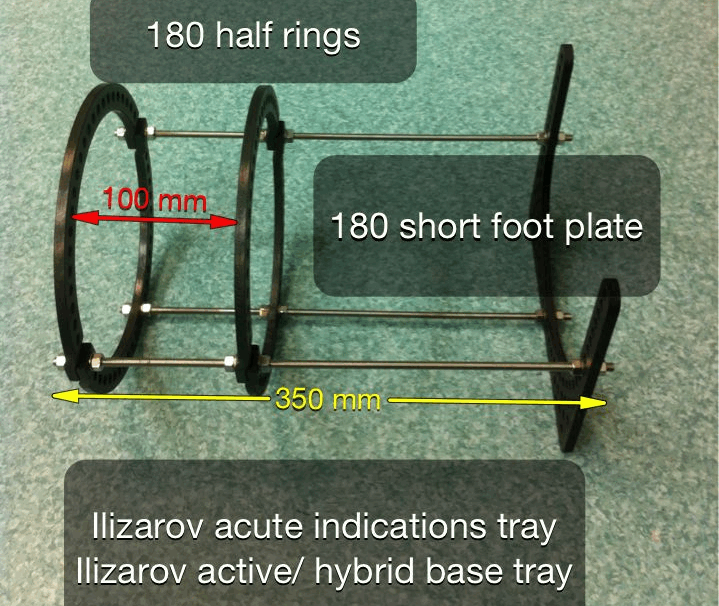 |
Look at the diameter of the patients calf, in general 180mm diameter
rings are good. Look at the length of the tibia and the proximal extent of the injury. You want your proximal rings and fixation points to be out of the zone of injury and away from future fixation options, eg medial tibial or anterior Tibial plate in Pilon fractures. Use between 350 to 400mm rods. A gap of 100-120 mm between the proximal rings just looks right. |
Pin sites
Proximal rings
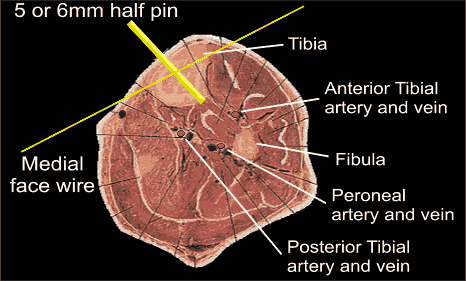 |
For the proximal
rings it is easiest to use hybrid of medial Tibial half pin 5 or 6mm on
a Rancho cube. Second point of fixation use medial face wire. |
Proximal medial half pins: Note the anterior tibial artery is anterior to the medial intermuscular septum, the posterior tibial artery lies posterior to Tibialis posterior, transfibular wires are not safe, drill carefully when doing the antero medial half pin
Place the medial face wire about 1cm lateral to the tibial crest and aim at
45 degrees, along the face to exit medially anterior to the posterior muscles
and the saphenous vein and nerve.
Number of fixation points on proximal rings depends on complexity of the injury and if it is temporary or definitive fixation. Use Ilizarov wires with +- an olive to pull tibia and provide counter balance points for three point fixation.
For the calcaneus use fine wires with considerations as above +- olives on the wires to pull the Calcaneus in the direction needed. Adjust traction on frame and pins on foot plate to reduce fracture.
I Don't usually for temporary external fixation reasons place fixation in the forefoot. The calcaneal wires sit behind the centre of rotation of the ankle and traction from the frame tends to dorsiflex the ankle. Ignore the look of the forefoot, look on the lateral the position of the Talus , ensuring it is plantigrade. Give the patient a towel, collar and cuff or strap to actively pull up foot.
If you need forefoot fixation use ilizarov wires through foot plate or build up rancho cube on foot plate.
A really powerful way to control the hind foot if needed is a schantz screw up the length of the calcaneus.
Post operatively
Dress pin sites
Elevate limb
Ensure regular pin site care
References
Traction and Orthopaedic Appliances; John D.M Stewart, Jeffrey P. Hallett
Percutaneous pin placement in the medial
calcaneus: is anywhere safe?
Casey D, McConnell T, Parekh S, Tornetta P 3rd.
J Orthop Trauma. 2004 Sep;18(8 Suppl):S39-42.
Personal thoughts: Lee Van Rensburg