Lumbar plexus block:
The lumbar plexus block targets three main nerves supplying the lower limb
which arise from the lumbar plexus.
This block is also called a
psoas compartment block. The three nerves which are targeted are
the
femoral, obturator and lateral femoral cutaneous nerve.
Anatomy:
The lumbar plexus is formed from the anterior primary rami of L1 – 4. In
50% of subjects it receives a contribution from T12.
The plexus gives rise to 3 small nerves (iliohypogastric, ilioinguinal
and genitofemoral) and 3 larger ones (femoral, obturator and lateral
femoral cutaneous nerve or LFCN) which are responsible for the nerve supply
of the lower limb.
The 3 larger nerves pierce the body of psoas major.
The LFCN and femoral
nerve emerge on the lateral border of psoas major and pass under the
inguinal ligament.
The obturator nerve leaves on the medial border of psoas muscle.
The following picture is from Gray's anatomy taken from wikimedia commons.
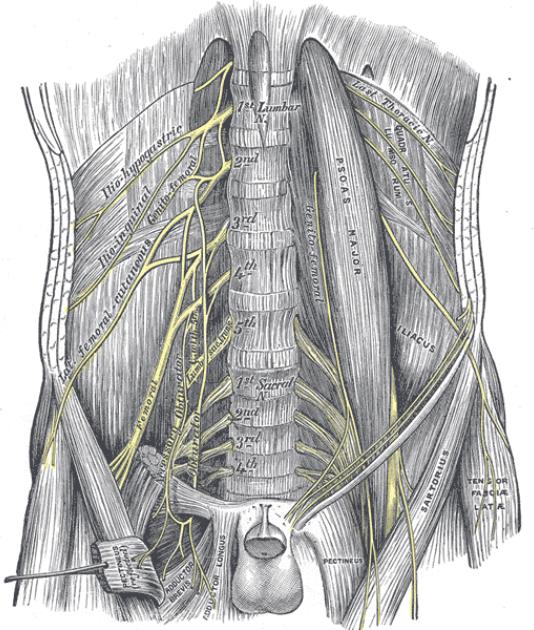
This picture shows on the left side of the body the relations of the nerve
with the psoas muscle and inguinal ligament. On right side the psoas
and inguinal ligament are removed.
The nerves lie in the posterior 1/3rd of the psoas muscle.
Indications:
1. The main indication is surgery on hip joint (e.g. hip replacement,
surgery for fracture neck of femur).
Contra-indications:
1. Patient refusal
2. Previous back surgery
3. Bleeding diathesis
4. Infection
Key points:
1. The lumbar plexus block is associated with some of the most life
threatening complications like total spinal anaesthesia, local
anaesthetic toxicity and damage to retroperitoneal structures.
Therefore this block should not be done without a proper indication.
There are other ways to provide pain relief to patients undergoing hip
replacement surgery.
2. The lumbar plexus block is better at providing complete blockade of the
lumbar plexus compared to a femoral three in one block and thus is a
very good block for the elderly population with fracture neck of femur.
Complete blockade provided by a lumbar plexus block in this population
reduces opioid requirement dramaticaly in the perioperative period.
3. Good knowledge of anatomy is very important with all blocks BUT this
is one of the blocks where not knowing the anatomy can have deadly
consequences.
4. Never use a needle longer than 10 cm.
5. If the going gets weird then stop- Tew's law i.e. if you are unable
to locate the lumbar plexus with reasonable effort, stop. Do not persists as
you are likely to do serious damage.
Necessary equipment:
1. Ultrasound machine with curvilinear probe, probe cover and ultrasound
gel
2. Insulated stimulating needle (I use 100 mm stimulating needle).
3. Local anaesthetic: I use 30 ml of 0.25-0.5% levobupivacaine
4. 2% chlorhexidine
Locating the lumbar plexus:
Unlike the peripheral nerves or the brachial plexus, it is very
difficult to see the lumbar plexus in all patients using ultrasound.
One of the ways we use ultrasound is to assist the nerve stimulator
guided lumbar plexus block.
Using anatomical landmarks (as
described by Capdevilla et al) the insertion point of the needle is
determined and marked as shown in the animation below.
Once the insertion point is marked the ultrasound is used to find out the
accuracy of the insertion point.
Ultrasound is used to find out:
1. Level of intervertebral interspace the insertion point corresponds
to.
2. Is it overlying the transverse process of the vertebra?
3. How deep is the transverse process from the skin?
4. Where is the lower pole of the kidney?
5. How deep is the peritoneum and the bowel from the skin?
The following video illustrates this point:
Once the above has been determined then the lumbar plexus block is done
using a nerve stimulator.
In my experience the lumbar plexus can
usually be found within 2-3 cm deeper of tranverse process (e.g. if the
transverse process is at 5cm from skin then you should expect the lumbar
plexus to be between 7-8cm from the skin.)
A 10 cm needle is inserted with no medial (towards spine) or lateral
angulation. If the transverse process is encountered then the needle is
walked off the transverse process either in cephalad or caudal
direction.
When the needle is in an ideal position then quadriceps
twitches are seen.
Local anaesthetic is injected after a sensible
threshold current (around 0.5mA) is obtained.
Complications:
1. Local anaesthetic toxicity
2. Damage to retroperitoneal structures e.g. kidney,bowel etc or
retroperitoneal haematoma
3. Total spinal anaesthesia
4. Death
Epidural spread of local anaesthetic is seen in around 6% of cases.
In the following video Dr Barry Nicholls expresses his views on Lumbar
plexus block and his technique of doing it.



