Interscalene block:
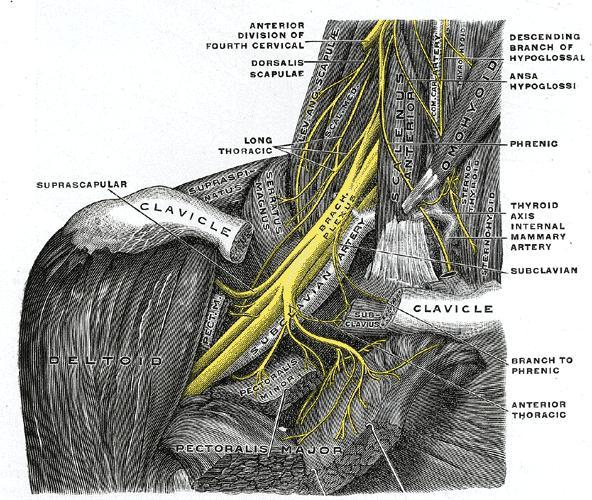
The interscalene approach to the brachial plexus
targets the roots of the brachial plexus as they emerge between
the scalene anterior and scalene medius muscle.
It is a useful block to
do for providing anaesthesia and analgesia for the shoulder and upper arm.
The important
neurovascular structures in the neck are quite close to target nerves.
Both these factors combine to make this the block with highest reported
publications of complications in the literature.
Anatomy
To understand the anatomy related to this block let us first see how the
brachial plexus is formed:
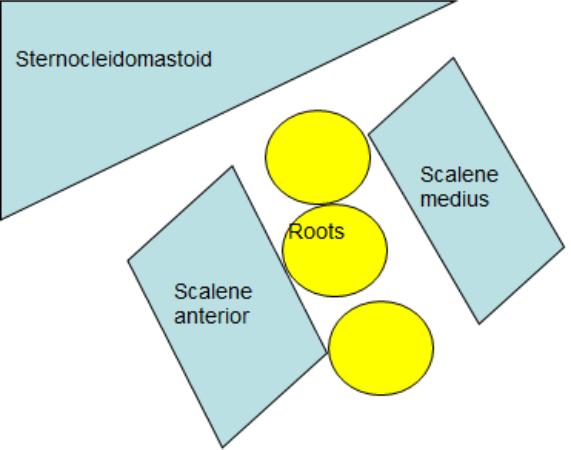
The roots of the brachial plexus emerge between the two scalene muscles
(scalene anterior and scalene medius).
In the interscalene groove
they lie on top (stack) of each other .
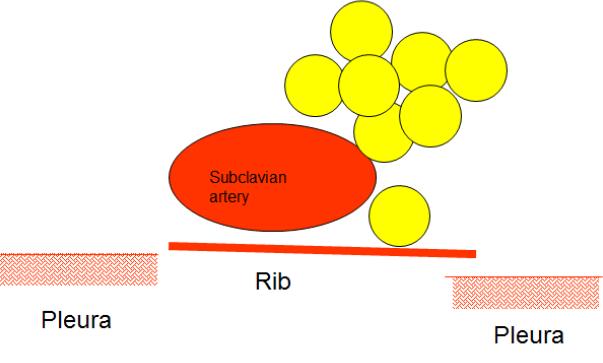
In the supraclavicular region the
roots form the trunks which lie posterior and superior to the subclavian
artery as it passess over the first rib.
To quote Dr Denny 'The brachial plexus can be likened to a vertical meat
baguette placed in the neck. The back of the baguette is the
Scalenus medius muscle. The front is the Scalenus anterior muscle, with
the roots and trunks of the plexus forming the meat or filling of the
sandwich or baguette, in between the 2 muscles, which insert onto the
first rib. It is long up and down and narrow front to back and not very
deep. In fact it is more like a filled baguette than a sandwich, which
rests on the first rib'.
Locating the nerves:
Start scanning in the supraclavicular fossa.
Position the probe
posterior to the clavicle so that a cross sectional view of the
subclavian artery is obtained.
You will notice the first rib inferior
to the artery.
It will be seen as a white line with a very dark
background. This is because rib does not allow any ultrasound to
pass through it but reflects all the ultrasound incident on it.
The periosteum of the rib appears as a white hyperechoic line with darkness
behind it as no ultrasound reaches it.
You will also notice the pleura
on either side of the rib, inferior to it.
The pleura is seen as a
shimmering white line (comet tail appearance).
The trunks of the
brachial plexus will be seen as bunch of grapes posterior and superior
to the subclavian artery.
Once the above has been identified start scanning cephalad keeping
nerves in the centre of picture.
You will see that the nerves
which are bunched up behind the subclavian artery in the supraclavicular
fossa stack up on top of each other as the probe is moved cephalad.
The scalene anterior and scalene medius muscle lie on each side of the
nerves with sternocleidomastoid lying over the nerve roots.
As the roots are traced cephalad they will be seen disappearing
into the vertebra.
The video below explains this further:
Other nerves in the neck that can be identified are Dorsal scapular
nerve, phrenic nerve, suprascapular nerve, superficial cervical plexus,
supraclavicular nerves and the greater auricular nerve.
To see these
nerves a high end machine with a high frequency linear transducer is
needed.
To successfully perform an interscalene block it is not
necessary to visualise all these nerves.
Dorsal scapular nerve:
This nerve will be seen crossing the substance of scalene medius
muscle.
The following video shows this nerve passing through the substance of
scalene medius muscle.
This video also shows the spinal accessory nerve.
During in plane approach to the roots of the brachial plexus as the
needle passess through the scalene medius muscle there is a possibility
of this nerve getting damaged.
Suprascapular nerve:
In the neck the suprascapular nerve can be seen arising from the C5 root as it is traced towards
the supraclavicular fossa.
The following video shows the suprascapular
nerve arising from C5.
Indications:
Surgery on shoulder, upper arm and lateral elbow.
Contraindications:
1. Patient refusal
2. Coagulopathy
3. Infection at the block site.
4. Respiratory compromise: Interscalene block has potential to cause
blockade of the phrenic nerve (almost 90% of cases) thus leading to hemidiaphragmatic paresis.
This is poorly tolerated in patients who have pre-existing respiratory
compromise.
In these patients interscalene block should be avoided
and an alternative block should be used like doing suprascapular nerve block
for pain relief.
Necessary Equipment:
1. Ultrasound machine with high frequency probe, probe cover and
ultrasound gel
2. Insulated stimulating needle (I use 50 mm stimulating needle).
3. Local anaesthetic: I use 20 ml of 0.5% levobupivacaine if block is
done for anaesthesia. For postoperative analgesia 0.25% levobupivacaine
is also sufficient
4. 2% chlorhexidine
Performing the block:
Keep the patient supine with 45 degrees head up.
Position the arm
as shown in the picture.
Stand at the head end on the side of
shoulder to be blocked and position the machine on the opposite side.
Start scanning in the supraclavicular fossa. Identify the
subclavian artery.
Look posterosuperior to the artery for the
trunks of the brachial plexus. Trace the trunks
cephalad till the nerve roots are seen stacked up on top of each other.
I use 50 mm insulated needle connected to the nerve stimulator.
Nerve stimulator is set at 1mA, 2 Hz.

The needle is introduced in-plane so that the entire needle is visualised as it
approches the roots.
I aim to have the ultimate position of the needle
between the C5 and C6 nerve root.
At this point either a biceps or a
deltoid twitch is observed.
The current is then reduced till
threshold current between 0.3-0.5 mA is achieved and local anaesthetic is injected as shown
in the animation below.
I combine ultrasound with nerve stimulation but
my colleagues do the block only using ultrasound.
There is no evidence
to suggest that combining the techniques improves safety.
If the
needle position is ideal even if the threshold current is high I inject
local anaesthetic and observe it's spread.
The following video shows an interscalene block being done. This video is by
'Nerve Imaging Group' and can also be seen on RA-UK website.
Useful
References:
Classified according to
1.Approach used to perform Interscalene block
2.Needle Angle
3.Nerve identification
4.Local anaesthetic used
5.Adjuvants
6.Volume of local anaesthetic
7.Catheter
Approach
Classic Winnie
Winnie AP. Interscalene brachial plexus block. Anesthesia and analgesia
1970; 49 (3): 455-466.
Pippa technique (posterior approach)
Pippa P, Cominelli E, Marinelli C, Aito S. Brachial plexus block using
the posterior approach. Eur J Anaesthesiol 1990;7:41120
Meier technique
Meier G, Bauereis C, Heinrich C. Interscalene brachial plexus catheter
for anesthesia and postoperative pain therapy. Experience with a
modified technique. Der Anaesthesist 1997; 46: 7159. (often quoted but
unable to locate a copy in English hence used reference below)
Peripheral Regional Anesthesia: An Atlas of Anatomy and Techniques.
Gisela Meier, Johannes Buettner. Thieme Medical Publishers. Aug 2007
Lateral modified
Borgeat A, Ekatodramis G: Anaesthesia for shoulder surgery. Best Pract
Res Clin Anaesthesiol 2002; 16:21125
Borgeat A, Dullenkopf A, Ekatodramis G, Nagy L. Evaluation of the
lateral modified approach for continuous interscalene block after
shoulder surgery. Anesthesiology 2003; 99: 43642.
Paravertebral approach
Boezaart AP, Koorn R, Rosenquist RW. Paravertebral approach to the
brachial plexus: an anatomic improvement in technique. Reg Anesth Pain
Med 2003;28:241
Posterolateral approach
Nguyen HC, Fath E, Wirtz S and Bey T. Transscalene Brachial Plexus
Block: A New Posterolateral Approach for Brachial Plexus Block. Anesth
Analg 2007;105:8725
Needle angle
Sardesai A, Patel R, Denny NM, et al. Interscalene brachial plexus
block: can the risk of entering the spinal canal be reduced? A study of
needle angles in volunteers undergoing magnetic resonance imaging
Anesthesiology 2006; 105: 913.
K. E. Russon, M. J. Herrick, B. Moriggl, H. J. Messner, A. Dixon, W.
Harrop-Griffiths and N. M. Denny. Interscalene brachial plexus block:
assessment of the needle angle needed to enter the spinal canal.
Anaesthesia, 2009, 64, pages 4345
Nerve identification
Prelocation
Urmey WF, Grossi P. Percutaneous electrode guidance: a non-invasive
technique for prelocation of peripheral nerves to facilitate peripheral
plexus or nerve block. Reg Anaesth Pain Med 2002; 27: 2617
Nerve stimulator
Baracco E, Verardo T, Scardino M, Geddo E. Brachial plexus block via the
interscalene route. The value of a nerve stimulator. Apropos of 38
cases. Cahiers dAnesthesiologie 1992; 40: 4379
Liguori GA, Zayas VM, YaDeau JT, Kahn RL, Paroli L, Buschiazzo V, Wu A.
Nerve localization techniques for interscalene brachial plexus blockade:
a prospective, randomized comparison of mechanical paresthesia versus
electrical stimulation. Anesth Analg 2006;103:7617
Ultrasound
Perlas A, Niazi A, McCartney C, Chan V, Xu D, Abbas S. The sensitivity
of motor response to nerve stimulation and paresthesia for nerve
localization as evaluated by ultrasound. Reg Anesth Pain Med 2006; 31:
445 50
Sinh SK, Abrams JH, Weller RS. Ultrasound-guided interscalene needle
placement produces successful anesthesia regardless of motor stimulation
above or below 0.5 mA. Anesthesia Analgesia 2007; 105: 84852.
Orebaugh SL, Williams BA, Kentor ML. Ultrasound guidance with nerve
stimulation reduces the time necessary for resident peripheral nerve
blockade. Regional Anesthesia and Pain Medicine 2007; 32: 44854.
Kapral S, Greher M, Huber G, et al. Ultrasonographic guidance improves
the success rate of interscalene brachial plexus blockade. Regional
Anesthesia and Pain Medicine 2008; 33: 253-258
Liu SS, Zayas VM, Gordon MA, C. Beathe JC, Maalouf DB, Paroli L, Liguori
GA, Ortiz J, Buschiazzo V, Ngeow J, Shetty T, Ya Deau YT. A Prospective,
Randomized, Controlled Trial Comparing Ultrasound Versus Nerve
Stimulator Guidance for Interscalene Block for Ambulatory Shoulder
Surgery for Postoperative Neurological Symptoms. Anesth Analg
2009;109:26571
Spence BC, Beach ML, Gallagher JD and Sites BD. Ultrasound-guided
interscalene blocks: understanding where to inject the local
anaesthetic. Anaesthesia, 2011, 66, pages 509514
McNaught A, Shastri U, Carmichael N, Awad IT, Columb M, Cheung J, Holtby
RM and McCartney CJL. Ultrasound reduces the minimum effective local
anaesthetic volume compared with peripheral nerve stimulation for
interscalene block. British Journal of Anaesthesia 2011; 106 (1): 12430
Local anaesthetic
Al-Kaisy AA, Chan VWS, Perlas A. Respiratory effects of low-dose
bupivacaine interscalene block. Br J Anaesth 1999; 82: 217 220
Borgeat A, Kalberer F, Jacob H, Ruetsch YA, Gerber C. Patient-controlled
interscalene analgesia with ropivacaine 0.2% versus bupivacaine 0.15%
after major open shoulder surgery: the effects on hand motor function.
Anesthesia and Analgesia 2001; 92: 21823.
Borghi B, Facchini F, Agnoletti V, A.Adduci, A.Lambertini, E.Marini,
P.Gallerani, V.Sassoli, M.Luppi and A Casati. Pain relief and motor
function during continuous interscalene analgesia after open shoulder
surgery: a prospective, randomized, double-blind comparison between
levobupivacaine 0.25%, and ropivacaine 0.25% or 0.4%. European Jourrnal
of Anaesthesiology 2006; 23: 10059.
Adjuvants
Dexamethasone
Effect of dexamethasone on the duration of interscalene nerve blocks
with ropivacaine or bupivacaine. K. C. Cummings III, D. E. Napierkowski,
I. Parra-Sanchez, A. Kurz, J. E. Dalton, J. J. Brems and D. I. Sessler
British Journal of Anaesthesia 2011; 107 (3): 44653
Clonidine
Culebras X, Van Gessel E, Hoffmeyer P, Gamulin Z. Clonidine combined
with a long acting local anaesthetic does not prolong postoperative
analgesia after brachial plexus block but does induce hemodynamic
changes. Anesth Analg 2001; 92: 199204.
Marco Nadig, Georgios Ekatodramis, and Alain Borgeat. What to Do with
Clonidine with Long-Acting Local Anesthetic in Brachial Plexus Block?
Anesth Analg July 2002 95:254
Opioid
Flory N, Van-Gessel E, Donald F, et al. Does the addition of
morphine to brachial plexus block improve analgesia after shoulder
surgery? Br J Anaesth 1995;75:236.
Volume of local anesthetic
Al-Kaisy A, McGuire G, Chan VW, Bruin G, Peng P, Miniaci A and Perlas A.
Analgesic effect of interscalene block using low-dose bupivacaine for
outpatient arthroscopic shoulder surgery. Regional Anesthesia and Pain
Medicine 1998; 23: 46973.
S. Riazi, N. Carmichael, I. Awad, R. M. Holtby and C. J. L. McCartney.
Effect of local anaesthetic volume (20 vs 5 ml) on the efficacy and
respiratory consequences of ultrasound-guided interscalene brachial
plexus block. British Journal of Anaesthesia 2008; 101 (4): 54956
Stimpson J, Carter J, Denny N. Interscalene Block and Phrenic Nerve
Palsy. Br J Anaesth 2008; 16 November 2008.
Renes SH, Rettig HC, Gielen MJ, Wilder-Smith OH, van Geffen GJ.
Ultrasound-guided low-dose interscalene brachial plexus block reduces
the incidence of hemidiaphragmatic paresis. Reg Anesth Pain Med 2009;
34: 498 502
Catheter
Tuominen M, Pitkanen M, Rosenberg PH. Postoperative pain relief and
bupivacaine plasma levels during continuous interscalene brachial plexus
block. Acta Anaesthesiologica Scandinavica 1987; 31: 2768.
Posterior approach
Boezaart AP, de Beer JF, du Toit C, van Rooyen K. A new technique of
continuous interscalene nerve block. Canadian Journal of Anaesthesia
1999; 46: 27581. (also describes benefit of using nerve stimulator)
Modified lateral approach for catheter insertion
Alain Borgeat, M.D., Alexander Dullenkopf, M.D., Georgios Ekatodramis,
M.D., Ladislav Nagy, M.D. Evaluation of the Lateral Modified Approach
for Continuous Interscalene Block after Shoulder Surgery. Anesthesiology
2003; 99:436 42
Tuohy needle
N. M. Denny, N. Barber and D. J. Sildown. Evaluation of an insulated
Tuohy needle system for the placement of interscalene brachial plexus
catheters Anaesthesia, 2003, 58, pages 554557
Ultrasound guided catheter placement
Fredrickson MJ. The sensitivity of motor response to needle nerve
stimulation during ultrasound guided interscalene catheter placement.
Regional Anesthesia and Pain Medicine 2008; 33: 2916.
Fredrickson MJ, Ball CM, Dalgleish AJ. A prospective randomized
comparison of ultrasound guidance versus neurostimulation for
interscalene catheter placement. Regional Anesthesia and Pain Medicine
2009; 34: 5904.
Fredrickson MJ, Ball CM, Dalgleish AJ, Stewart AW, Short TG. A
prospective randomized comparison of ultrasound and neurostimulation as
needle end points for interscalene catheter placement. Anesthesia and
Analgesia 2009; 108: 1695700.
Ilfeld BM, Fredrickson MJ, Mariano ER. Ultrasound-guided perineural
catheter insertion: three approaches, but few illuminating data.
Regional Anesthesia and Pain Medicine 2010; 35: 565
Catheter and ambulation
Klein SM, Grant SA, Greengrass RA, et al. Interscalene brachial plexus
block with a continuous catheter insertion system and a disposable
infusion pump. Anesthesia and Analgesia 2000; 91: 14738.
Ilfeld BM, Morey TE, Wright TW, Chidgey LK, Enneking FK. Continuous
interscalene brachial plexus block for postoperative pain control at
home: a randomized, double-blinded, placebo- controlled study. Anesth
Analg 2003; 96: 108995
Sardesai AM, Chakrabarti AJ, Denny NM. Lower lobe collapse during
continuous interscalene brachial plexus local anesthesia at home.
Regional Anesthesia and Pain Medicine 2004; 29: 658.
Ilfeld BM, Vandenborne K, Duncan PW, Sessler DI, Enneking KF, Shuster
JJ, Theriaque DW, Chmielewski TL, Spadoni EH, Wright TW. Ambulatory
continuous interscalene nerve blocks decrease the time to discharge
readiness after total shoulder arthroplasty: a randomized,
triple-masked, placebo-controlled study. Anesthesiology 2006; 105:
9991007.
Fredrickson MJ, Ball CM, Dalgleish AJ. Successful continuous
interscalene analgesia for ambulatory shoulder surgery in a private
practice setting. Regional Anesthesia and Pain Medicine 2008; 33: 1228.
Hofmann-Kiefer K, Eiser T, Chappell D, Leuschner S, Conzen P, Schwender
D. Does patient-controlled continuous interscalene block improve early
functional rehabilitation after open shoulder surgery? Anesthesia and
Analgesia 2008; 106: 9916
Patient controlled Interscalene analgesia vs PCA Borgeat A, Schappi B,
Biasca N, Gerber C. Patient controlled analgesia after major shoulder
surgery. Patient controlled Interscalene analgesia versus patient
controlled analgesia. Anesthesiology 1997; 87: 1343.
Borgeat A, Tewes E, Biasca N, Gerber C. Patient controlled Interscalene
analgesia with ropivicaine after major shoulder surgery: PCIA vs PCA.
BJA 1998; 81: 603.
Continuous infusion versus patient controlled Singelyn FJ, Seguy S,
Gouverneur JM. Interscalene brachial plexus analgesia after open
shoulder surgery: continuous versus patient-controlled infusion.
Anesthesia and Analgesia 1999; 89: 121620. .



