Axillary block
The axillary approach to the brachial plexus targets the four terminal braches of
the brachial plexus namely median, ulnar, radial and Musculocutaneous nerves.
One of the widely practiced blocks done by anaesthetists, emergency physicians
and surgeons.
Apart from blood vessels and nerves there are not many vital
structures in this region (e.g. cervical spine, viscera etc). Provided
intravascular injection is avoided this block is very safe to perform.
It does
however, have a significant failure rate with non-ultrasound methods.
This is
due to the fact that:
1. The nerves are not close together like in the supraclavicular fossa where
the trunks are tightly packed together and a single injection can block all the
trunks.
The musculocutaneous nerve leaves the plexus within the axilla and is
separated from the other three nerves in the axilla.
The other three nerves even
though they are closer to the artery, their position around the artery is quite
variable as will be discussed later.
2. The fascial sheath that surrounds the axillary neurovascular bundle is not
continuous.
There are definite septae and attachments within this sheath which
restrict free flow of the local anaesthetic deposited in the sheath.
Anatomy:
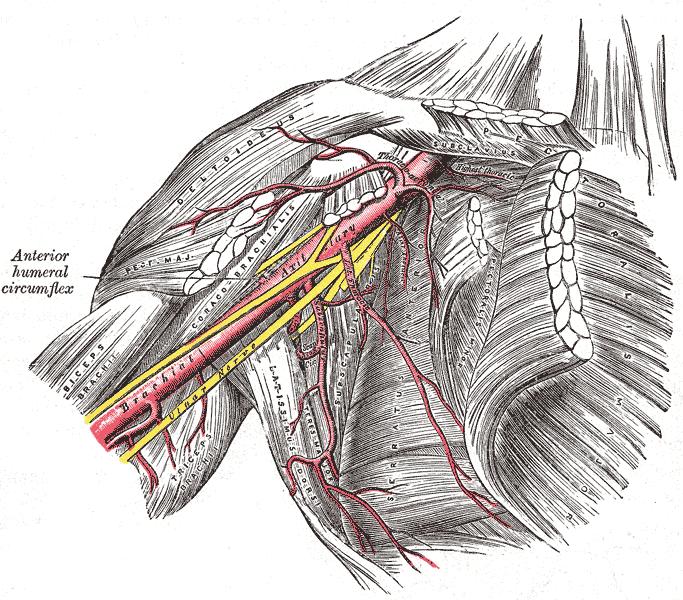
The above picture is from Gray's anatomy.
The
axilla is a pyramidal shaped region situated between the chest wall and the
upper arm.
The chest wall forms the medial boundary and the humerus the lateral
boundary.
Superiorly lies the pectoral fold.
Latissimus dorsi forms the
inferior boundary.
The neurovascular bundle running through axilla consists of
the Axillary artery, vein/s, and terminal branches of brachial plexus.
The
Musculocutaneous nerve in most cases lies superior to the artery in the coracobrachialis muscle.
The other three nerves lie around the artery.
The position of the other three nerves in relation to the Axillary artery is highly variable.
This is shown in the diagram below.
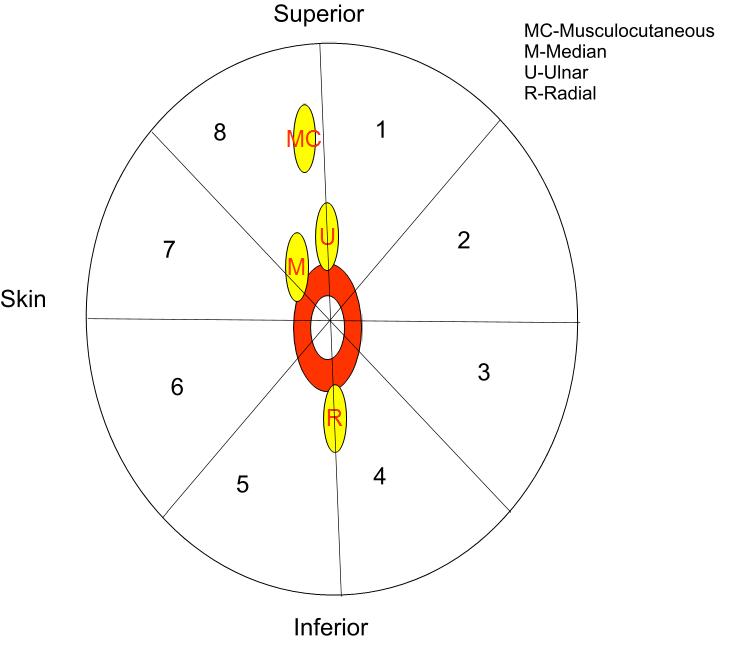
Imagine that the person being scanned is supine. The arm is abducted at the
shoulder, elbow flexed and forearm supinated.The probe is placed over the
axilla such that a cross sectional view of the axilla is obtained.
Following is a diagrammatic representation of the ultrasound image.
In this diagram the space around the
Axillary artery (Red circle in the centre) is divided into 8 pie chart sectors.
The median nerve is found most of the time superior and anterior (nearer the
skin) to the Axillary artery in region 6,7and 8.
The ulnar nerve can be seen in
region 1, 2 and 3 (Inferior and anterior to artery).
The radial nerve in the
region 2, 3, 4 and 5 (posterior to artery and inferior).
The regions indicate
where the nerve can be found mostly.
It is possible for the nerves to lie
anywhere else as well.
Indications:
1. Surgery on the elbow, forearm and hand.
Contraindications:
1. Patient refusal
2.
Coagulopathy, although if this is the only anaesthetic you can give to a patient
due to his medical problems then this block can be done with minor coagulopathy
as blood vessels can be easily compressed to stop bleeding.
3. Infection at
the site of the block.
Key points:
1. There are four nerves to be blocked
and they are not close to each other. Therefore a single nerve injection is
unlikely to block all nerves.
2. The musculocutaneous nerve always needs to be
blocked separately as it is not enclosed in the so called axillary sheath. It
needs to be blocked to prevent tourniquet pain.
3. The arm is not a perfect
cylinder and nerves do not travel in a straight line in it. In order to get the
best picture of the nerve the probe will have to be angled cephalad and caudal and
rotated clockwise and anticlockwise.
4. Look for the structure which can be
easily identified first i.e pulsating blood vessels. Then look for the nerves
as detailed in locating the nerves in relation to them.
Necessary Equipment:
1. Ultrasound machine with high frequency probe, probe cover and ultrasound
gel
2. Insulated stimulating needle (I use 50 mm stimulating needle).
3. Local anaesthetic: I use 20
ml of 0.5% levobupivacaine if block is done for anaesthesia. For postoperative
analgesia 0.25% levobupivacaine is also sufficient
4. 2% chlorhexidine
Locating the nerves:
The patient is supine. The arm is abducted at the
shoulder, elbow flexed and forearm supinated.
The ultrasound machine and the
operator are positioned as shown in the picture:
A linear high frequency
ultrasound probe is used.
The probe is placed as high in the axilla under the
pectoral fold.
The probe is placed such that cross sectional view of the artery
is obtained.
To start with do not make any attempt to identify the nerves.
Find the structure that you can easily identify.
That will be the axillary
artery which will be seen as a pulsating structure which cannot be compressed.
Once the axillary artery is identified ease the pressure off the probe and you will
see the axillary vein filling up. After
the vascular structures are
identified then look for the nerves.
As discussed before the position of the nerves in relation to the artery is
variable.
Median Nerve
Keep the artery in the centre of picture and scan from the axilla towards the elbow.
You will see a nerve which stays with the artery all the time.
It starts
superiorly (usually) and around midarm level crosses over the artery to lie on
its medial side.
This is the median nerve.
Ulnar nerve:
Once you have found the median nerve, go back to the axilla
and focus your attention on finding the ulnar nerve.
Start in axilla and
follow the artery down towards the arm.
This time keep the artery in
upper part of the screen. Just above the midforearm level you will see a
structure breaking away from the inferior side of the artery going away.
It lies above the muscles and just underneath the subcutaneous plane.
As you follow it down towards the elbow it seems to be heading towards the
medial epicondyle and then at the elbow seems to go behind the medial epicondyle
( so called ‘Sun set’ sign). This is the ulnar nerve.
Radial nerve:
The radial nerve although with
the axillary artery in the axilla, it
sharply breaks away from it to go behind the humerus in the spiral groove to
emerge four finger breadths above the lateral epicondyle and then it travels in the
groove between biceps and brachioradialis muscle.
To start looking for the radial nerve start in the axilla and then scan towards elbow.
You will see a band or a ribbon shape or a railtrack like structure breaking
away from the axillary artery going towards the humerus.
If you follow it back towards the axilla you will see it resting between the
axillary artery and triceps muscle.
Musculocutaneous nerve:
At the level of the axilla, the musculocutaneous nerve is meant
to lie in the substance of coracobrachialis muscle.
It has a very shiny appearance It is oval in shape. It normally
seems to dive between the muscle planes like a fish.
There is considerable
variation in anatomy of musculocutaneous nerve.Francis Remerand et.al. (Anesth Analg 2010;110:1729–34)
have described the variation very nicely. They studied all the patients
undergoing ultrasound guided axillary block between Dec 2006 and Dec 2008.
They found that the musculocutaneous nerve was outside the coracobrachialis
muscle in 22% of cases. It was near the axillary artery
in 6% of patients. The musculocutaneous and median nerves appeared as a common
neural structure in 16% of individuals studied.
Tracing back the radial nerve:
Following video also shows how to find nerves for axillary block
Performing the nerve block:
This block needs to be performed in-plane.
The needle
tip has to be visualized at all times. The patient lies supine with arm abducted at
the shoulder, elbow flexed and forearm supinated.
The anaesthetist sits/stands
at the head end of the patient with ultrasound machine positioned opposite him
as shown in the picture.
This is the most ergonomic position for
doing the block. We use 50 mm insultaed needle.
We combine ultrasound with
nerve stimulation. Median, ulnar and musculocutaneous nerves are quite easily
visible . The radial nerve can sometimes be tricky.
Try to surround the nerves with
local anaesthetic, aim to block all four nerves (If you can’t find all four
nerves block at least three out of four nerves; always block the
musculocutaneous nerve, other two neves depending on the site of surgery).
You
can always block median, ulnar and radial nerves more distally. Locate and
block the nerves as discussed before.
Please check this video from RA-UK website. You will see Dr Nigel Bedforth
expertly doing an axillary block on Dr James French. Both are Consultant
Anaesthetist at Nottingham, UK. Video courtesy ‘Nerve Imaging Group’. It
works best on a PC.
Iphone/ipad and mobile users
click here
References:
1) Ultrasonographic Findings of the Axillary Part of the Brachial Plexus. Gerald Retzl et.al. Anesth Analg 2001;92:1271–5
2) Efficacy of Ultrasound-Guided Axillary Brachial Plexus Block: A Comparative Study with Nerve Stimulator-Guided Method. Fu-Chao Liu et.al. Chang Gung Med J 2005;28:396-402
3) A Prospective, Randomized Comparison between Ultrasound and Nerve Stimulation Guidance for Multiple Injection Axillary Brachial Plexus Block. Andrea Casati et.al. Anesthesiology 2007; 106:992– 6
4) Ultrasound guidance improves success rate of axillary brachial plexus block. Vincent W.S. Chan et.al. CAN J ANESTH 2007 / 54: 3 / pp 176–182
5) A Comparison Between Ultrasound-Guided Infraclavicular Block Using the “Double Bubble” Sign and Neurostimulation-Guided Axillary Block. De Q. H. Tran .et.al. Anesth Analg 2008;107:1075–8
6) Assessment of topographic brachial plexus nerves variations at the axilla using ultrasonography.J.-L. Christophe. et.al. British Journal of Anaesthesia 2009; 103 (4): 606–12
7) Is the Musculocutaneous Nerve Really in the Coracobrachialis Muscle When Performing an Axillary Block? An Ultrasound Study. Francis Remerand et.al. Anesth Analg 2010;110:1729–34
8) A Clinical Evaluation of Block Characteristics Using One Milliliter 2% Lidocaine in Ultrasound-Guided Axillary Brachial Plexus Block. Brian O’Donnell et.al. Anesth Analg 2010;111:808–10



