Supraclavicular block:
With this approach to the brachial plexus the trunks of the plexus are
blocked as they cross the first rib.
The brachial plexus at this
point is most compact along it's course. An injection of local
anaesthetic at this level has a good chance of blocking the entire
plexus.
Before use of ultrasound to do nerve blocks became common, this block
fell out of favour due to the risk of causing pneumothorax.
Ultrasound has made this block popular again.
Anatomy:
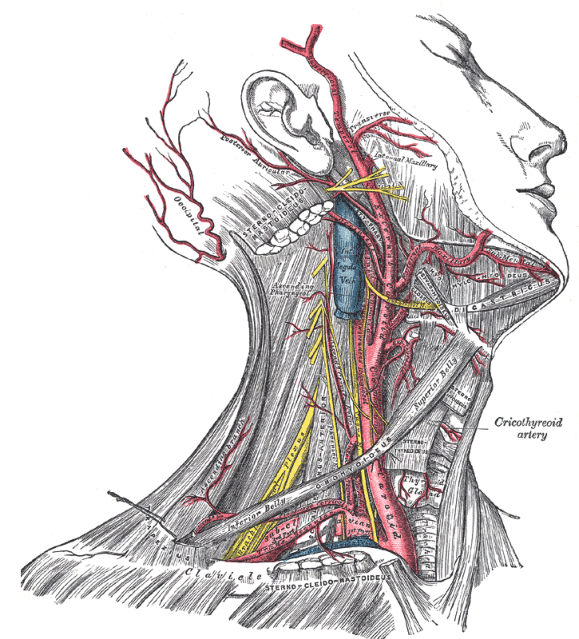
The roots of the brachial plexus emerge between the two scalene muscles,
scalene anterior and scalene medius. The Scalene muscles originate from the
cervical transverse processes and insert on the first rib.
The plexus
crosses the first rib between the insertions of the anterior scalene
muscle (in front) and the middle scalene (behind).
At this level
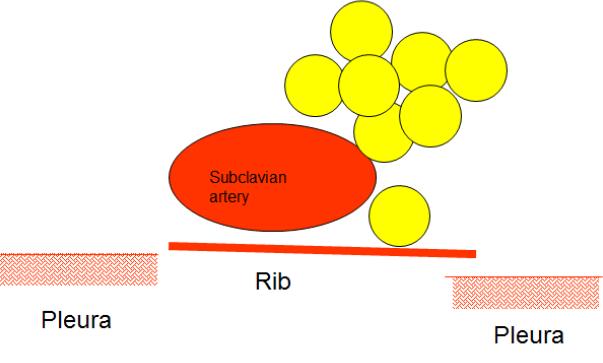
the roots have divided to form the trunks. The trunks lie
posterior and slightly superior to the subclavian artery as it passess
over the first rib.
The lower trunk may lie between the subclavian
artery and the first rib.
Locating the nerves:
Place the probe in the
supraclavicular fossa. Do not attempt to look for the nerves.
First find the subclavian artery. Once you have found the subclavian
artery find the best cross section view of the artery.
When that
is accomplished then look posterior and superior to the artery for the
trunks of the brachial plexus. The trunks will be bunched up.
You will see first rib below the subclavian artery. It will be
seen as a white hyperechoic line with darkness behind it. Pleura
will be seen on either side of the rib below it.
The pleura has a
'comet tail' appearance. Unlike the rib you see a lot of
shimmering behind the pleura.
Indications:
1. Good for humeral, elbow, fore-arm and hand surgery.
Not a good block for surgery confined to the medial side of the hand or
the little finger as the inferior trunk can often be missed .
Contraindications:
1. Patient refusal
2. Coagulopathy
3. Infection at the site of the block.
4. Emphysematous chest.
Necessary Equipment:
1. Ultrasound machine with high frequency probe, probe cover and
ultrasound gel
2. Insulated stimulating needle (I use 50 mm stimulating needle).
3. Local anaesthetic: I use 20 ml of 0.5% levobupivacaine if block is
done for anaesthesia. For postoperative analgesia 0.25% levobupivacaine
is also sufficient 4. 2% chlorhexidine
4. Nerve stimulator
Performing the block:
Keep the patient supine with 45 degrees head up. Position the arm as
shown in the picture.

Stand at the head end on the side of shoulder to be blocked and position
the machine on the opposite side. Start scanning in the supraclavicular
fossa. Identify the subclavian artery. Look posterosuperior to the
artery for the trunks of the brachial plexus. Identify the pleura.
Use colour doppler to find any branches of subclavian artery amongst the
trunks of the brachial plexus.
Once this is done the needle is introduced in plane so that it is
visualised at all times.
The block is done as shown in the
animation.
This video shows block being done as described in the animation.
The following video shows a supraclavicular block being done. This video is
by 'Nerve Imaging Group' and can also be seen on RA-UK website
A parasagittal approach to brachial plexus has been described by Dr
Searle et al. In this approach with the patient in supine position with
his head turned to opposite side, high frequency linear probe is placed
in the parasagittal plane so as to obtain a cross sectional view of the
subclavian artery lying over the first rib. The plexus is seen
posterior to it. Needle is introduced in plane to lie in the
sheath of the plexus. Local anaesthetic is injected to fill the
sheath. Needle is redireced if the spread of local
anaesthetic is inadequate. The advantage of this approach as
suggested in the paper is less risk of pneumothorax as the needle stays
above the first rib (therefore away from pleura) all the time.
The paper is available to view freely on the
internet.
We have described ultrasound guided nerve block above but following is
video of Dr Herrick describing how to do nerve stimulator guided
subclavian perivascular nerve block.



