Combined Suprascapular Nerve and Axillary Nerve Block:
Interscalene block is used to provide analgesia after shoulder surgery
as it blocks most of the sensory nerves coming from the shoulder area
(except T2 and sometimes the superficial cervical plexus). However
interscalene block almost invariably leads to phrenic nerve palsy which
in some cases can lead to respiratory compromise. Some patients do
not like feeling of numb arm. Some frightening complications have
been reported following interscalene block like tetraplegia and total
spinal.
Although interscalene block is the gold standard when it comes to
providing analgesia following shoulder surgery, there are alternatives
available.
Combined block of the suprascapular and axillary nerve block has been
described as an alternative by Price.1 This so called
'Shoulder block' provides analgesia following shoulder surgery.
This has to be part of multimodal pain relief technique as unlike
interscalene block some degree of residual pain is to be expected.
Suprascapular Nerve:
Anatomy:
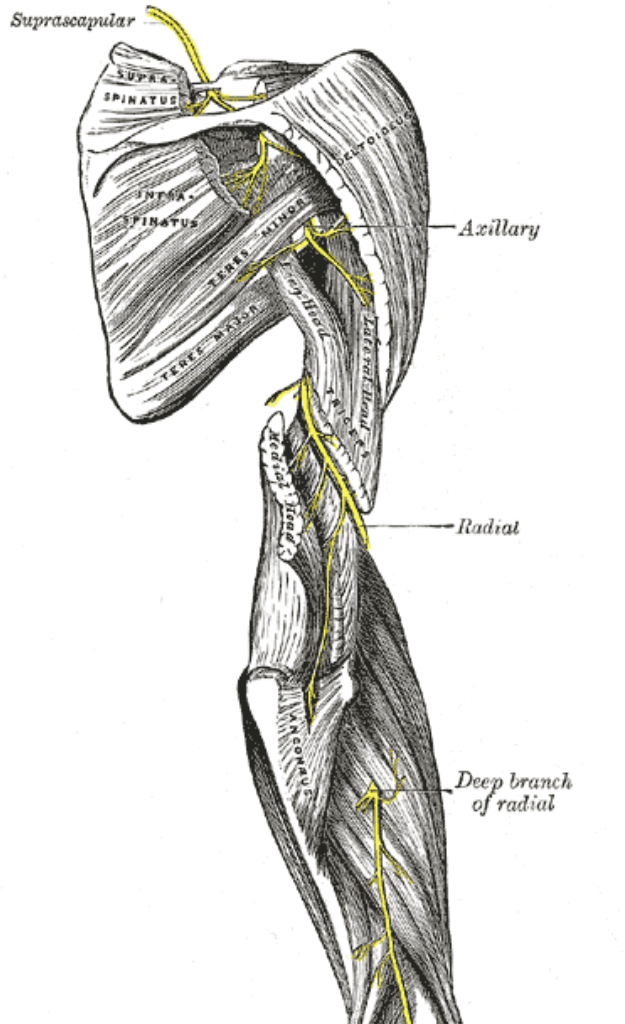
The suprascapular nerve is a branch of upper trunk
which is formed by union of C5 and C6 nerve root.
It passes under the trapezius and omohyoid muscle laterally to
enter the supraspinatus fossa.It does that by passing through suprascapular notch under the
superior transverse scapular ligament.
It then passes under the supraspinatus muscle giving a branch to
it and an articular branch to shoulder joint.It then goes around the lateral border of spine of scapula to
enter the infraspinatus fossa.In here it gives branches to infraspinatus muscle and the
shoulder joint.
As the nerve passes under the transverse scapular
ligament it is accompanied by suprascapular artery which passes over the
ligament (mnemonic to remember this: Army above navy below .
Imagine a bridge over a river.Army will go over the bridge to cross it while the navy will go
under that bridge.
Following video demonstrates the anatomy of the suprascapular nerve. With kind permission of Prof Len funk
Locating suprascpular nerve using ultrasound:
Following video shows how to locate the suprascapular nerve using
ultrasound. Scanning started just above and parallel to the spine
of the scapula.
Indications:
Analgesia for surgery on shoulder with or without block of the axillary nerve
Contraindications:
1. Patient refusal
2. Coagulopathy
3. Infection at the block site.
Necessary Equipment:
1. Ultrasound machine with high frequency probe, probe cover and ultrasound gel
2. Insulated stimulating needle (I use 100 mm stimulating needle).
3. Local anaesthetic: I use 10 ml of 0.5% levobupivacaine if block is done for anaesthesia. For postoperative analgesia 0.25% levobupivacaine is also sufficient
4. 2% chlorhexidine
Performing the block:
Patient is positioned as shown in the picture.
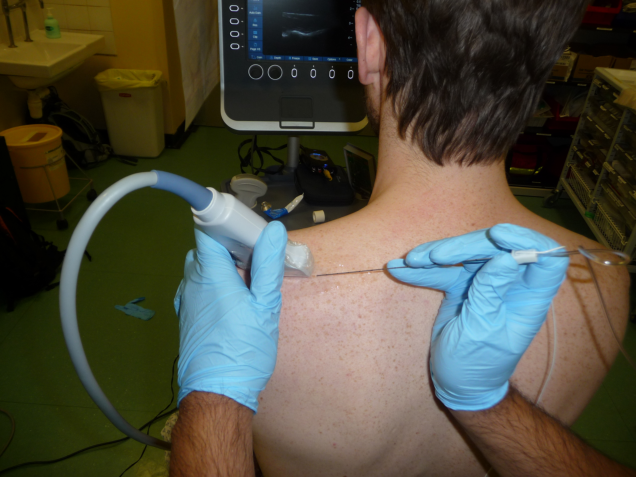
We use 100 mm needle and not the 150 mm neeedle shown in the picture. A 50 mm needle will be useful as well but 100 mm is more convenient to come in plane. Trick is not to go too deep and visualise the needle all the time.Needle is introduced in plane either from medial to lateral or lateral to medial side. If a stimulator is used then you will see slight external rotation and abduction of the shoulder. After threshold current is established 10 ml of 0.5% levobupivacaine is injected.
Axillary Nerve Block
This is not axillary brachial plexus block which blocks median, radial, ulnar and musculocutaneous nerves but a block of the axillary nerve.
Anatomy:
Axillary nerve is a branch of posterior cord. Axillary nerve first lies behind the axillary artery then winds around the humerus accompanied by posterior humeral circumflex artery.It emerges through quadrilateral space. Quadrilateral space is bound superiorly by subscapularis and teres minor. Inferior boundry is made by teres major. Long head of triceps forms the medial boundary while surgical neck of humerus lies laterally. Axillary nerve then divides into into an anterior, a posterior, and a branch to the long head of the triceps brachii.
Locating the nerve:
Following video shows how to locate the nerve.
Scanning started around midarm level posteriorly. Look for shadow produced by the humerus in the ultrasound picture. Follow it towards the shoulder. You will see the shadow curving upwards as the probe approaches the head of the humerus.
Indications:
Analgesia for surgery on shoulder with suprascapular nerve block.
Contraindications:
1. Patient refusal
2. Coagulopathy
3. Infection at the block site.
Necessary Equipment:
1. Ultrasound machine with high frequency probe, probe cover and ultrasound gel
2. Insulated stimulating needle (I use 100 mm stimulating needle).
3. Local anaesthetic: I use 10 ml of 0.5% levobupivacaine if block is done for anaesthesia. For postoperative analgesia 0.25% levobupivacaine is also sufficient
4. 2% chlorhexidine
Performing the block:
Patient is positioned as shown in the picture.

The needle is inserted in plane. We use 100 mm needle and not the 150 mm neeedle shown in the picture. If a stimulator is used then you will observe twitching of the deltoid muscle. After threshold current is established 10 ml of 0.5% levobupivacaine is injected.
References:
1. Price DJ. The shoulder block: a new alternative to interscalene brachial plexus blockade for the control of postoperative shoulder pain. Anaesth Intensive Care 2007 Aug;35(4):575-81.
2. Harmon D, Hearty C. Ultrasound-guided suprascapular nerve block technique. Pain Physician. 2007;10:743-746.
3. Peng PWH, Wiley MJ, Liang J, Bellingham GA. Ultrasound-guided suprascapular nerve block: a correlation with fluoroscopic and cadaveric findings. Can J Anesth. 2010;57:143-148.
4.Gorthi V, Moon YL, Kang JH. The effectiveness of ultrasonography-guided suprascapular nerve block for perishoulder pain. Orthopedics. 2010;16:238-241.
5.Chan CW, Peng PW. Suprascapular nerve block: a narrative review. Reg Anesth Pain Med. 2011 Jul-Aug;36(4):358-73.
6.Rothe C, Asghar S, Andersen H L, Christensen JK, Lange KHW. Ultrasound-guided block of the axillary nerve:
a volunteer study of a new method. Acta Anaesthesiol Scand 2011; 55: 565–570.



